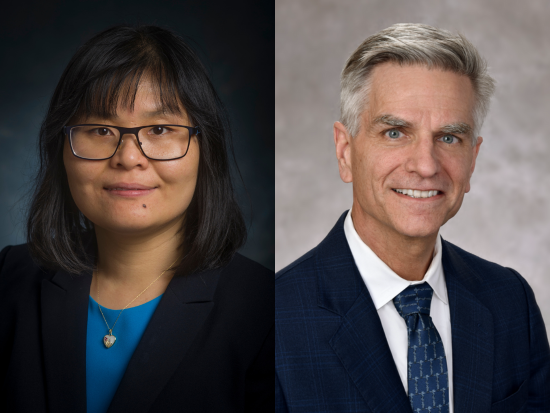
 The University of Alabama at Birmingham Department of Neurosurgery Associate Professor Jianmei Leavenworth, M.D., Ph.D., and James Garber Galbraith Endowed Chair of Neurosurgery James Markert, M.D., MPH, are among the authors of a recent study published in Nature Communications that explores the use of modified oncolytic viruses (OVs) as a potential therapy for glioblastoma multiforme (GBM), one of the most aggressive and fatal forms of brain cancer.
The University of Alabama at Birmingham Department of Neurosurgery Associate Professor Jianmei Leavenworth, M.D., Ph.D., and James Garber Galbraith Endowed Chair of Neurosurgery James Markert, M.D., MPH, are among the authors of a recent study published in Nature Communications that explores the use of modified oncolytic viruses (OVs) as a potential therapy for glioblastoma multiforme (GBM), one of the most aggressive and fatal forms of brain cancer.
The study, titled “Oncolytic reprogramming of tumor microenvironment shapes CD4 T-cell memory via the IL6ra-Bcl6 axis for targeted control of glioblastoma,” investigates the impact of an oncolytic herpes simplex virus (oHSV) engineered to express interleukin-12 (IL-12), a protein known for its ability to enhance the immune system’s response against tumors.
While previous research has demonstrated that OVs—when modified—can attack and destroy cancer cells, scientists do not yet fully understand how these viruses affect the tumor environment over time or how well the immune system continues fighting long-term after treatment.
A need for new treatment
GBM, the most common and aggressive malignant glioma in adults, remains a significant challenge among patients and healthcare providers. Despite current standard-of-care treatments, including surgical tumor resection, chemotherapy and radiation, there is a median survival of just 12 to 15 months from initial diagnosis and as little as four to six months after recurrence. The challenges in treating GBM stem from its immunosuppressive tumor microenvironment, which enables cancer cells to evade the body’s immune system and continue growing.
To address this, researchers have turned to immunotherapy—a strategy that enhances the natural immune response against cancer. Oncolytic virotherapy, in particular, involves genetically modifying viruses to selectively infect and kill cancer cells while also activating an immune response against tumors.
Researchers at UAB have examined how a modified oHSV expressing IL-12 could be used to stimulate the immune system and improve long-term tumor control.
Key findings
During the study, researchers found that CD4 T cells, a subset of immune cells, were essential in maintaining long-term tumor control following treatment with the engineered oHSV.
After treatment, researchers observed an upregulated major histocompatibility complex class II (MHCII) on residual tumor cells, which allowed the immune system to remain primed for future attacks and “remember” the cancer, ensuring a quick and aggressive response if the tumor returned.
The study found that for these immune cells to work properly with an enhanced anti-tumor capacity, they needed the proper ratio of Bcl-6 to T-bet expression, which plays a crucial role in the development and function of immune cells.
The research highlighted the necessity of a reciprocal IL6ra-Bcl-6 regulatory axis within memory CD4 T cells, which requires MHCII signals from reprogrammed tumor cells, tumor-infiltrating and resident myeloid cells, for a prolonged and effective immune response.
Implications for future GBM treatment
For patients diagnosed with GBM, which accounts for approximately 30% of primary brain tumors in adults in the United States, advancements in treatment options are urgently needed.
The findings of this study reinforce the potential of oncolytic virotherapy not only as a direct tumor-killing mechanism but also as a means of "training" the immune system to recognize and combat tumors more effectively in the future.
By leveraging immunotherapy, researchers in the Department of Neurosurgery hope to develop more effective treatments for glioblastoma that will lead to higher survival rates and better outcomes for patients.
“The implications of this research are significant,” said Leavenworth, who also serves as the assistant program leader for the O’Neal Comprehensive Cancer Center’s Cancer Biology and Immunology Program. “By demonstrating how an engineered oncolytic virus can reshape the tumor environment and enhance long-term immune cell memory, we are moving closer to therapies that will not only eliminate tumors but also prevent their recurrence.”
Other authors of this study include Jeffrey Grimes, Ph.D., as first author, Sadashib Ghosh, Ph.D., Shamza Manzoor, MS, Li, Li, M.D., Ph.D., Monica Moran, Jennifer Clements, MPH, and Sherrie Alexander, MA.
For more information, refer to the full study in Nature Communications.