XENOTRANSPLANT
UAB researchers establish optimal immunosuppression regimen for pig-to-human kidney transplants

The regimen — which includes already FDA-approved medications, plus the use of a complement inhibitor — showed remarkable success in Parsons model case series.
Xenotransplant is defined as transplanting an animal organ or product into a human to cure disease. Utilizing genetically modified pig kidneys could provide an increased supply for those needing a kidney transplant.
Why do we need xenotransplantation?
“We have this amazing therapy called kidney transplantation that works 95 to 98 percent of the time, and yet there are only about 25,000 kidneys to go around in the U.S. every year, but we have 800,000 people who need them. The hardest part is seeing patients in clinic and wait-listing them knowing they might actually die before I ever get an organ-offer to transplant them.
So the opportunity to have an organ that is waiting there for the person who needs it is just overwhelming to think about. I feel very privileged to be just a tiny part of a really big puzzle that people have been working on for many years.”
- Dr. Jayme Locke, Director, Division of Transplantation,
Heersink School of Medicine
UAB advances the science in 2023
-

New study: Pig kidneys — for the first time — demonstrate “life-sustaining kidney function” in a human
This study, performed in a pre-clinical human model, is the first time xenotransplanted pig kidneys have shown clearance of creatinine and shown a standard immunosuppression regimen may be sufficient.Read how we’re advancing the science30185 views
Read more about UAB’s 2022 breakthrough
-

Pig kidneys to humans: next steps for the UAB xenotransplantation program
UAB physicians are working on the next steps to begin compassionate or emergency use of the pig kidneys in living humans. Two major approvals will be required.What’s on the horizon for xenotransplantation?18844 views
UAB announces first clinical-grade transplant of gene-edited pig kidneys into brain-dead human
In the study published in the American Journal of Transplantation, UAB researchers tested the first human preclinical model for transplanting genetically modified pig kidneys into humans.Why did UAB publish this study?48934 views
Selfless act paves the way for more people to receive lifesaving organs
Jim Parsons’ legacy paves the way for thousands to potentially receive lifesaving organs through UAB’s xenotransplantation program.The Parsons family and their gift21511 views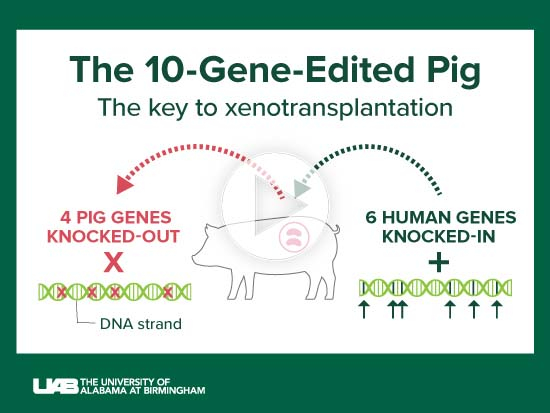
The 10-gene pig and other medical science advances enabled UAB’s transplant of a pig kidney into a brain-dead human recipient
The human preclinical model at UAB provides important knowledge before a Phase I clinical trial can begin for living human recipients. Decades of work by researchers across the world preceded UAB’s first clinical-grade pig kidney xenotransplant.The science behind the study30204 views
Pig-to-human kidney transplant one of many feats for Locke, UAB Comprehensive Transplant Institute
From its incompatible kidney transplant program to deceased donor programs, to xenotransplantation, UAB continues to seek ways to help patients who face end-stage renal disease.Meet Jayme Locke, M.D.14386 viewsLearn more about this research
Photos of the UAB Xenotransplant Team
UAB’s breakthroughs in the news
-
Pig organs for transplant patientsNouvelle greffe d’un rein de porc chez un humain aux États-UnisKidneys From a Genetically Altered Pig Are Implanted in a Brain-Dead Patient
Media resources for journalists
Media Kit
Assets, including photos, videos, graphics and press releases, are available for media to download.
Resources for mediaEDITOR’S NOTE: The University of Alabama at Birmingham is one of three doctoral research universities in the University of Alabama System. In your first reference to our institution, please use University of Alabama at Birmingham and UAB on subsequent references.

















