 UAB's Xenotransplant team. (From left, front row: Jayme Locke, M.D., Katie Stegner, Lindsey Banks, Amy Johnson, M.D., Sara Macedon;Back row: Babak Orandi,M.D., Ph.D., Jordan Lee, M.D., Paige Porrett, M.D., Ph.D., Brett Findley, Natalie Budd, Douglas Anderson, M.D., Drew Shunk, M.D., JennyAnn Eads)
UAB's Xenotransplant team. (From left, front row: Jayme Locke, M.D., Katie Stegner, Lindsey Banks, Amy Johnson, M.D., Sara Macedon;Back row: Babak Orandi,M.D., Ph.D., Jordan Lee, M.D., Paige Porrett, M.D., Ph.D., Brett Findley, Natalie Budd, Douglas Anderson, M.D., Drew Shunk, M.D., JennyAnn Eads)
Photo taken by Steve Wood, UABOnce Jayme Locke, M.D., made the decision to become a transplant surgeon, all she has ever wanted to do is save lives.
In the field of kidney transplant surgery, that leads to many great triumphs, and also heartbreaking disappointment.
“The hardest part is seeing patients in clinic, putting them on a transplant waitlist and knowing that they might die before I even get an organ offer to be able to transplant them,” said the 45-year-old Locke, who is the director of the University of Alabama at Birmingham’s Comprehensive Transplant Institute in the UAB Marnix E. Heersink School of Medicine.
Locke hopes another door to save the lives of patients in end-stage kidney disease has been kicked down with the Jan. 20, 2022, peer-reviewed publication in the American Journal of Transplantation of a xenotransplantation study performed Sept. 30, 2021, at UAB Hospital and Legacy of Hope, Alabama’s organ procurement organization.
Locke’s research team transplanted two genetically modified pig kidneys inside the abdomen of a brain-dead human after removing the recipient’s native kidneys; the transplanted kidneys filtered blood, produced urine and, importantly, did not reject. Details of the study can be found here.
This first-of-its-kind accomplishment is potentially a monumental step forward for the future of kidney transplantation. And it may mean Locke and other transplant surgeons will soon be able to transplant patients with end-stage kidney disease faster than ever before.
“I could not be more excited for my patients or more proud of what our UAB transplant team accomplished with this study,” Locke said. “As transplant surgeons, we have a gold standard available to us in kidney transplantation. It’s a therapy that, if it were a chemotherapeutic agent, everyone’s minds would be blown. A kidney transplant works 95 to 98 percent of the time. There are very few therapies for the treatment of a disease that are that effective. And it’s curative for an end-stage disease. You’re taking someone who has an end-stage problem, meaning the end of the line, and if you don’t fix this problem for them, they are going to die.
Videography: Jeff Myers and Steve Wood
Produced by: Andrea Reiber and Tyler Greer
“So, the opportunity, the notion, the concept of being able to literally have an organ on the shelf that is just waiting there for the person who needs it is remarkable to think about. It’s exciting for our patients. I feel very privileged to be a very tiny part of a really big puzzle that people have been working on for many, many years.”
Many UAB scientists and researchers past and present have contributed to this moment that the university believes will enhance what is already one of the United States’ most robust, successful and innovative kidney transplant programs — with Locke and her contemporaries leading the way.
Only the University of California-San Francisco has performed more kidney transplants than UAB since statistics began being kept on Jan. 1, 1988. In fact, from Jan. 1, 1988, through Dec. 31, 2021, UAB performed 9,055 kidney transplants, according to the United Network for Organ Sharing, including almost 3,435 living donor transplants.
Locke is the surgical director of the South’s leading Incompatible Kidney Transplant Program at UAB Hospital and coordinator of the UAB Kidney Chain, which is the longest living kidney-transplant chain ever recorded in the United States, with 126 donors and recipients. These programs, along with the Hepatitis-C positive to negative deceased donor and HIV-positive to positive deceased donor programs, demonstrate UAB’s commitment to finding alternative avenues to achieve transplant for those in need.
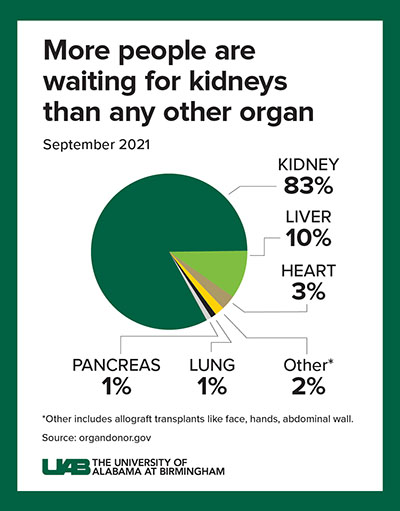
Click image to enlarge
Graphic: Jody Potter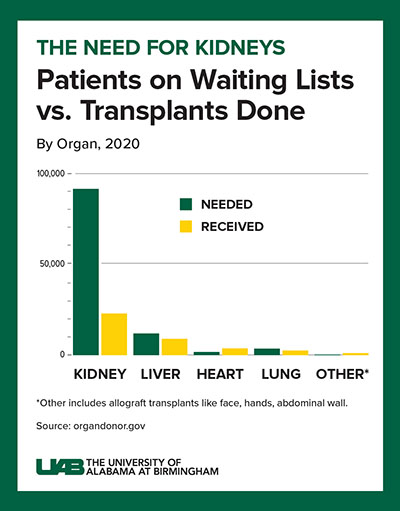
Click image to enlarge
Graphic: Jody PotterThere is a need. A 2019 study from Health Testing Centers found that Alabama is the state with the longest wait time for organ transplants in the nation. It also found that almost 31 percent of Alabamians in need of a kidney transplant had been on the waiting list for more than five years. Approximately 1,200 Alabamians are currently awaiting a kidney transplant. More than 800,000 Americans nationwide live with kidney failure. However, kidney transplantation remains elusive, despite efforts to increase the donor pool. Fewer than 25,000 kidney transplants are performed each year in the United States, and 240 Americans on dialysis die every day. Many of these deaths could be prevented if an unlimited supply of kidneys were available for transplant.
Finding innovative ways to help patients get to transplant faster has been a focus for UAB researchers and physicians for decades.
“Without question, UAB is 100 percent committed to our patients,” Locke said. “End-stage disease in Alabama is a huge problem. Our residents face high rates of end-stage kidney disease. UAB’s commitment to help figure out creative ways to find more organs — whether it be getting behind the incompatible kidney transplant program and expanding living donation, or launching the Hep-C positive into negative deceased donor program, or in this case, making substantial investments and building out a xenotransplantation program that involves developing and building a pathogen-free facility where these animals can be raised so we can ensure we don’t transmit any viruses to humans from these animals — is remarkable. It’s a testament to UAB’s commitment to our community, our patients and the betterment of the human condition.”
More than a decade ago, UAB’s kidney transplant program began laying the groundwork to build a paired exchange and incompatible transplant program that would help patients who are difficult to match. New technologies emerged that enabled researchers and clinicians to specifically define harmful antibodies that are present in many previously transplanted patients.
DID YOU KNOW You can be a living kidney donor? Call 888-822-7892 or visit uabmedicine.org/kidneytransplant to find out how. To indicate your interest in donating your organs after death, visit www.organdonor.gov and sign up today.
“Our translational research program at UAB is robust, innovative and one of the best in the nation,” said Selwyn Vickers, dean of the UAB Heersink School of Medicine and CEO of the UAB Health System and UAB/Ascension St. Vincent’s Alliance. “Achieving a successful xenotransplant — which is critical in developing a sustainable and viable opportunity for all patients in need — was a bold goal we set in 2016 when United Therapeutics provided funding to really launch our program. The work of our researchers to achieve this in five years has been tremendous. And Dr. Locke and her surgical team also deserve a lot of credit for ensuring the success of the study by completing this transplant and seeking to solidify its success through peer-reviewed, published research. Alabama is fortunate to have a highly skilled, highly driven surgeon-scientist like Dr. Locke leading our Comprehensive Transplant Institute. She works tirelessly for her current and future patients, and this is further proof.”
With this xenotransplant study complete, UAB researchers and surgeons can begin to look forward to what comes next — which will hopefully be a Phase I clinical trial to perform a xenotransplant into a living human.
“Life is in so many ways miraculous,” Locke said. “The ability to have but a small part of helping to give that gift is both humbling and exhilarating. To look in someone’s eyes and see hope restored is an amazing feeling. My wish is that xenotransplantation will give us another way to restore hope for many others.”