By: Erica Techo
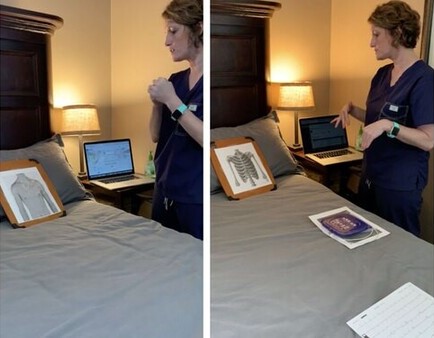
A Tupperware container, phone charger, clear tape and a cutting board. These are just a few of the things Assistant Professor Summer Powers, CRNP, ACNP-BC, AACC, needs for a virtual EKG.
You might not believe it, but these everyday household items can simulate an EKG for a virtual skills validation, and the idea came from faculty’s innovative thinking and a few notes from Pinterest.
“Our skills check-offs are usually performed in person, but when we learned that the semester would finish in a remote setting, I worked to adapt the process,” Powers said. “Students have most of the correct equipment in their nursing skills kits necessary to do EKG and other skills check-offs from home, but some left their kits on campus before going home for spring break. I wanted to make sure everyone could adapt their skills check-off at home with what they had on hand, including a printable copy of the thorax or ribs.”
Powers also worked with the School’s Instructional Technology team and fellow colleagues to record instructional videos for students, so they knew exactly how to do the skill set-up and demonstrated the video checkoffs for students. These videos were loaded in their Canvas course shell.
Students recorded their own checkoffs through the camera on their phone or computer and submitted a final video through the online GoReact system, which allows instructors to review and give feedback on student performance.
While the remote experience was different from a usual in-person skills validation, Powers said the students not only showed adaptability in a remote setting — they also showed their creativity in the process.
“When students turned in their videos, some had gone the extra mile — adding a face or hair to their patient, rather than just utilizing the printed thorax or chest that I provided,” she said.
Fourth semester student Aaron Hollis was one of those students. As a hands-on learner, Hollis said the transition to virtual learning has been difficult at times, but the support and patience of faculty made the transition manageable.
“Our instructors have been really great about reaching out, emailing us and making sure we get everything done,” Hollis said. “When I learned we would do validations with a video submission, it was kind of a mad panic of, ‘How am I going to get this done in a studio apartment that I share with two dogs?’”
After a few camera adjustments to avoid any clutter in the background, Hollis said he chose to draw a patient on paper.
“The faculty always say nursing is about treating the patient, and not treating the process, so I really felt like I needed a face on my patient so I could talk to them,” Hollis said. “I’m also a very kinesthetic learner and having a face on my patient felt more in-line with my learning style.”
Palmer Miller, also a fourth semester student, brought her skills bag home before spring break and was able to use her equipment for her checkoffs. While she missed using the School’s technology and manikins for checkoffs and practice, Miller said the chance to record herself helped her relax throughout the process.
“I was really lucky to have my equipment, but the ingenuity that went into Dr. Powers’ videos and her ‘how to’ descriptions were great,” Miller said. “There are definitely benefits to running through these procedures in person, but I’m thankful to have faculty that support us and have made this work for us remotely.”
Remote learning also meant faculty had to transition a patient code simulation to a virtual code assignment. Students watched a video of a code, reflected on what they saw and filled out a code flow sheet as if they were in the room.
“When students are practicing codes in our simulation labs, everyone wants a task that isn’t the documentation,” said Instructor Kathy Langley, MSN, CRNP, AGACNP-BC. “As someone who has been in many code situations in practice, I know that filling out the code flow sheet is one of the hardest things to do, but it is important because it helps record vital information about treatment and medication that can inform next steps in care. When we moved to remote instruction, the students had to take on that task and learned where to write things and where to put information, which is so important once they enter into practice. A virtual code also allowed them to pause, rewind and go at their own pace, which for many helped the learning and retention process.”
Virtual simulations have been helpful, Miller agreed, as they allow for more repetition of skills — and a chance to ask more questions.
“With remote learning, it’s been beneficial to have more simulation assignments, even with V-sims,” Miller said. “Since we can’t be in the room with patients, it’s a great way to get critical thinking applications, to learn from mistakes and to ask questions. You’re also able to practice again and again and learn from those steps.”
Both the faculty and students said while going to remote learning because of the novel coronavirus (COVID-19) pandemic for the spring and now summer semester is not ideal, the students still have hands-on learning experiences and, in many cases, extra skills practice and one-on-one faculty interactions that are providing excellent skills foundations as students move through the program.
“One of my favorite things to teach my students is how to be ‘gumby’ in health care, as it is a dynamic and constantly changing field,” Powers said. “This unprecedented event has given both faculty and students the opportunity and challenge to be innovative — thinking outside the box collaboratively to meet the common goal of learning safe practice for patient care.”