The 50th annual American Spinal Injury Association had a strong UAB flavor, prominently featuring multiple CEDHARS members at the gathering held from April 17-19 in Atlanta.
In addition to having a presentation, Dr. Yuying Chen, co-director of CEDHARS and director of the UAB National Spinal Cord Injury Statistical Center, was introduced as a member of the ASIA board of directors. ”I feel very honored to be a part of the board.”
Also recognized at the conference, Dr. Salma Aly, part of the NCHPAD data team, won the Mulcahey Award for the clinical outcomes research category, as given by the ASIA conference panelists.
Read about the abstracts and their presenters.
Inclusion of Non-Traumatic Spinal Cord Injury in Spinal Cord Injury Model Systems Database: One Center’s Experiences
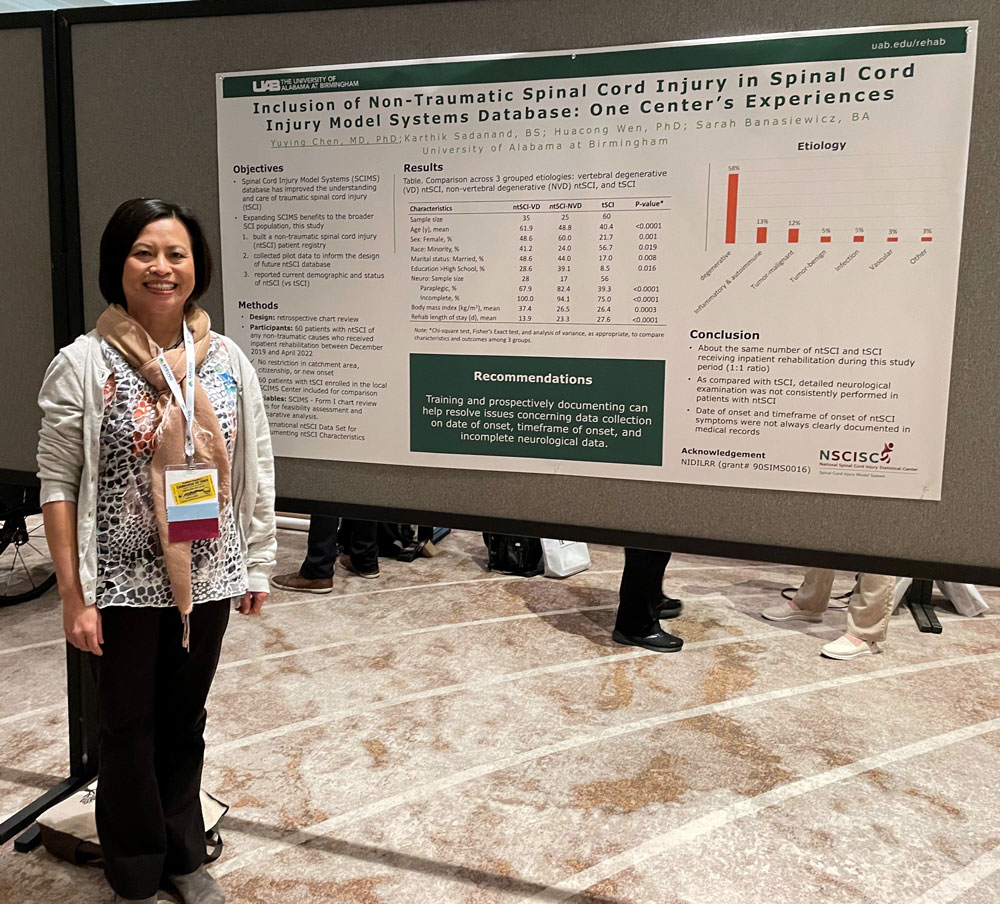 Presenter: Dr. Yuying Chen, director of research, Department of Physical Medicine and Rehabilitation
Presenter: Dr. Yuying Chen, director of research, Department of Physical Medicine and Rehabilitation
Collaborating Authors: Karthik Sadanand, BS; Huacong Wen, PhD; Sarah Banasiewicz, BA
Abstract
Objective: Research from Spinal Cord Injury Model Systems (SCIMS) National Database over the last 5 decades has contributed significantly to the understanding of traumatic spinal cord injury (tSCI) and improved the care of people with tSCI. The extent to which such knowledge and clinical practices applicable to people with non-traumatic spinal cord injury (ntSCI) is unclear. With an ultimate goal of expanding the benefits of SCIMS Database to the broader SCI population, this study was conducted to:
- build a ntSCI patient registry in parallel to the SCIMS Database,
- collect pilot data at a local SCIMS Center to inform the design of future ntSCI national database, and
- report current demographic trends and status of ntSCI.
Design/Methods: This study was a retrospective chart review of patients with ntSCI who received inpatient rehabilitation between December 2019 and April 2022. Data obtained mirrored the SCIMS - Form I chart review items for feasibility assessment and comparative analysis, including socio-demographic, neurological, and clinical information. International SCI Data Sets for ntSCI was used to document ntSCI characteristics. Patients with tSCI enrolled in the local SCIMS Center during the study period were included in the analysis. Chi-square test and analysis of variance were performed, as appropriate, to compare characteristics and outcomes among three grouped etiologies: tSCI, vertebral degenerative (VD) ntSCI, and non-vertebral degenerative (NVD) ntSCI.
Results: Among 60 patients with ntSCI enrolled, VD was the most common etiology (58.3%), followed by inflammatory (13.3%), neoplastic-malignant (11.7%), neoplastic-benign (5.0%), infection (5.0%), vascular (3.3%), and others (3.3%). During the study period, an identical number of patients with tSCI (n=60) were enrolled in the local SCIMS Database. People of VD etiology were older (61.9y) than those of NVD (48.8y) and tSCI (40.4y, p less than 0.001). Related to age differences, the majority of tSCI cases were single (64.4%) in comparison to VD (31.4%) and NVD (40.0%) groups (p = 0.008). VD cases were also heavier (body mass index [BMI]=37.4 kg/m2) than people of NVD (26.5 kg/m2) and tSCI (26.4 kg/m2, p less than 0.001). Most of people with tSCI were male (78.3%) and of minority race (56.7%), while the percentages were 51.4% and 41.2%, respectively, for VD and 40.0% and 24.0%, respectively, for NVD cases. Incomplete tetraplegia (48.2%) was the most frequent category in the tSCI group, while incomplete paraplegia was most common in the VD (67.9%) and NVD (82.4%) groups (p less than 0.001). Average length of rehabilitation stay was longest in the tSCI group (27.6 days), followed by NVD (23.3 days) and VD (13.9 days, p less than 0.001).
Conclusion: People with ntSCI of VD etiology were older and overweight, while those with tSCI had a higher level of injury and longer rehabilitation stay. As compared with tSCI, detailed neurological examination was not consistently performed in patients with ntSCI. Date and timeframe of onset of ntSCI symptoms were not always clearly documented. Training and prospectively documenting can resolve these issues. This study provides pilot data to guide the development of data collection protocol to include people with ntSCI in the future SCIMS Database.
Preliminary Findings for a Sequential Multiple Assignment Randomized Trial (SMART) to Increase Adherence to Home Exercise in People with Spinal Cord Injury (SCI): The SMART-HEALTH study
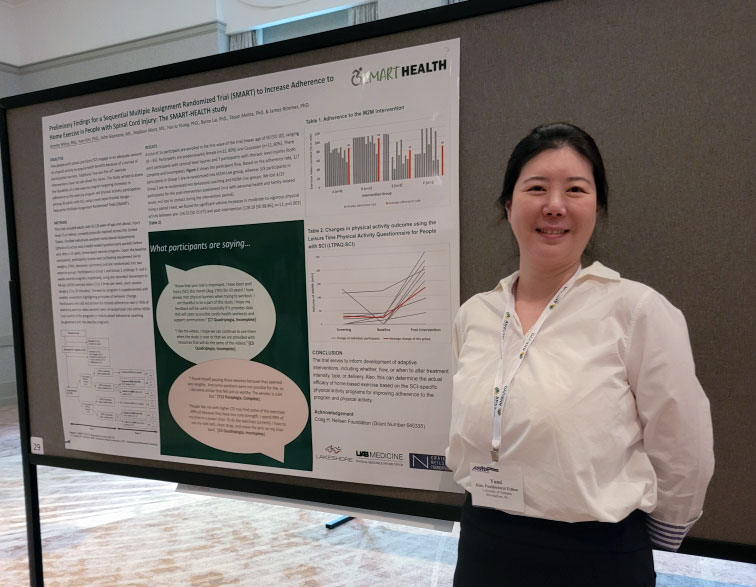 Presenter: Dr. Jereme Wilroy, co-director of the UAB Spinal Cord Injury Model System, director of research at Lakeshore Foundation, associate scientist in CEDHARS and a health behavioral specialist for NCHPAD.
Presenter: Dr. Jereme Wilroy, co-director of the UAB Spinal Cord Injury Model System, director of research at Lakeshore Foundation, associate scientist in CEDHARS and a health behavioral specialist for NCHPAD.
Collaborating Authors: Yumi Kim, PhD., John Giannone, MS., Madison Mintz, MS., Hui-Ju Young, PhD., Byron Lai, PhD., Tapan Mehta, PhD., James Rimmer, PhD.
“Our presentation appealed to a broad audience including healthcare providers and individuals with SCI in precision-based exercise programming and its delivery strategies,” Kim said. “We shared contact information for future collaborations. Also, we discussed the positive study findings with program officers from the Craig H. Neilsen Foundation (study sponsor) and the future direction and potential of this trial design.
Abstract
Our study aimed to assess the feasibility of a tele-exercise program targeting increased adherence to the exercise program and leisure time physical activity participation among 30 adults with SCI, using a novel experimental design – Sequential Multiple Assignment Randomized Trials (SMART). The first wave of this trial included 15 participants with a mean age of 50 years old [SD 10] and 6 cervical- and 7 thoracic-level injuries (both complete and incomplete). Participants were predominantly female (n=12, 80%) and Caucasian (n=12, 80%).
Based on the pre-determined criteria (> 95% of scheduled pre-recorded exercise video watch), 6 participants were re-randomized into either M2M-Live group (switched to 1x/week instructor-led program) or behavioral coaching group (augmented 1x/week coaching with the pre-recorded videos). Using a paired t-test, we found significant volume increases in moderate-to-vigorous physical activity (MVPA) between pre- (24.55 [SD 35.67]) and post-intervention (128.18 [SD 88.86]; n=11; p=0.003). Of those, 5 participants exceeded the mean MVPA value of the post-intervention, and 3/5 were re-randomized participants with low adherence at the beginning of the program. Our qualitative findings revealed participants’ positive experiences and perceptions toward the exercise program: “Know that your role is important. I have been post-injury for 43 years! I have always met physical barriers when trying to workout. I am thankful to be a part of this study. I hope my feedback will be useful especially if it provides data to open accessible cardio health workouts and support communities.” [C7 Quadriplegia.
Utilization of Machine Learning algorithm in prediction of hospital readmission during one-year post spinal cord injury
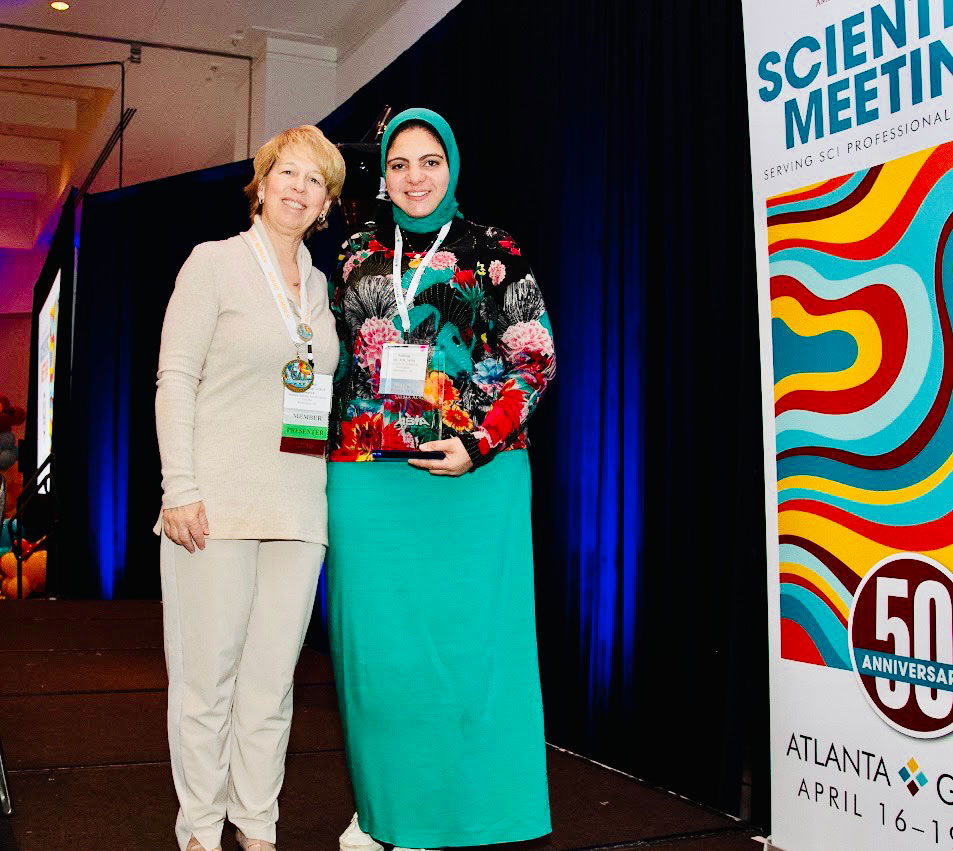 Presenter: Dr. Salma Aly, MD, MPH, data consultant, Department of Family and Community Medicine
Presenter: Dr. Salma Aly, MD, MPH, data consultant, Department of Family and Community Medicine
Collaborating Authors: Tapan Mehta, PhD, AbdulAziz Ahmed, PhD, Huacong Wen, MD, PhD, Yuying Chen, MD, PhD
“I won the Mulcahey award from ASIA conference which is a clinical outcome research award,” Aly said. “For me, it means that our research is applicable to clinical setting, and from perspective of the ASIA Panel, who gave me this award, they believe the our findings will be beneficial in modifying risk of rehospitalization after SCI.”
Abstract
Objective: The primary purpose was to generate a machine learning (ML) model to predict hospital readmission during 1-year post spinal cord injury (SCI) based on the patients’ assessments at the time of discharge from the rehabilitation center including demographic characteristics such as sex and residence, trauma etiology, age at injury, presence of associated injury or vertebral injury, use of any type of mechanical ventilation being used at time of discharge, the primary method of bladder management techniques, history of comorbidities as diabetes, hypertension, arthritis, and hyperlipidemia, history of depression or anxiety, Functional Independence Measure (FIM), level of neurological injury and ASIA Impairment Scale at Annual examination. The specific aim was to identify the top predictors for rehospitalization.
Design/Methods: Data were collected from the National Spinal Cord Injury Database which is submitted to the National Spinal Cord Injury Statistical Center (NSCISC) at the University of Alabama at Birmingham (UAB). Subjects will be those participants’ data from the pool of participants with a date of injury from 2011 till 2021. For our study, the subjects were divided into 2 groups, rehospitalization, and non-rehospitalization groups. The total sample was 4172 participants, out of them 1438 experienced rehospitalization during 1-year post-injury. Random oversampling was used to treat the class imbalance. Iterative-imputer was used for replacing missing data and one-hot encoding was used for dealing with categorical variables. The data was then split into 80% training data and 20% test data. Random oversampling is used to treat the class imbalance. Seven ML classification models (XGboost, Support vector machine (SVM), Random Forest (RF), logistic regression, Catboost, Decision tree (DT), and Naïve Bayes (NB)) were assessed to predict rehospitalization. Dimensionality reduction and feature selection were done using recursive feature elimination (RFE). The initial number of features included in the model was 98 and reduced to 48 features taking rank one by RFE. The SHAP method was used to interpret predictions. To control model overfitting, five-fold cross-validation was done.
Results: Out of the seven models tried, the XGBoost classification model was the best performing with the following evaluation metrics: average accuracy score of 75.5% ± 1.1%, F1 score equals 78.5% with sensitivity of 81.2%, and specificity of 72.3%. The area under the curve (AUC) was 76.7%. According to SHAP results, the top predictors in the model were age at the time of injury, residence in a group living situation, the performance of spinal surgery during initial rehospitalization, presence of associated injury, FIM score, and history of hyperlipidemia, arthritis, diabetes, and hypertension.
Conclusion: The XGBoost has a relatively high ability to rule in the patients who will be readmitted after SCI (81.2%) based on the assessment at the time of discharge from rehabilitation. Based on the SHAP values, older age at the time of injury, performing spinal surgery, having hyperlipidemia, arthritis, diabetes, and hypertension as comorbidities, and the presence of associated injury are considered to be risk factors for rehospitalization. On the other hand, the higher the FIM score, the lower the SHAP value so considered to be protective.
Work-related spinal cord injury (SCI): Does race/ethnicity matter?
Presenter: Dr. Huacong “Wendy” Wen, postdoctoral fellow, UAB Department of Physical Medicine and Rehabilitation
Collaborating Authors: Kyle Hsu, Michelle Turnley, MD, Jennifer Marwitz, MA
“I met other researchers and scientists who share same research interest,” Wen said. “I enjoyed this conference and learned a lot.”
Abstract
Objective: To investigate the racial differences in work-related injury among people with traumatic spinal cord injury (SCI)
Design/Methods: This was a cross-sectional analysis of data from National SCI Model Systems (SCIMS) database. There were 5,974 study participants (763 Hispanic, 1,478 Non-Hispanic Black, 3,484 Non-Hispanic White, and 249 other races) between the ages of 18-65 with SCI injured between October 2000 and December 2019. We compared the demographic characteristics, injury-related characteristics, and English language ability of the racial groups using the chi-square test or analysis of variance. Work-related injury was determined if the cause of SCI incurred in the course of employment. To assess the effect of race on work-related injury, logistic regression models were calculated by adjusting for demographic characteristics, injury-related factors, and English speaking ability. We also compared the occupational categories by racial groups among people with work-related injury using descriptive statistics, including frequencies and percentage.
Results: Significant differences across racial groups were noted for demographics, injury-related factors, and English language ability across racial groups. Compared to other racial groups, Hispanics tended to be younger, less educated men with less English-speaking ability and a higher rate of falls as the cause of injury. Work-related injuries were found to occur in 9.7% of the sample (n=581) with Hispanics having a higher percentage than other racial groups (15.6%, P less than 0.001), especially among those who are male (17.8%, P less than 0.0001) or injured by falls (41.5%, P less than 0.0001). When accounting for demographic and injury-related factors (sex, marital status, education, age, cause of injury, and severity of SCI), Hispanic people still had a higher likelihood of work-related injury when compared with non-Hispanic Black people (Odds ratio 1.59, 95% Confidence interval (CI) 1.12-2.24). After accounting for English speaking ability (self-rated from “not at all” to “very well”), the odds of work-related injury decreased to 1.254 (95% CI 0.87-1.82). Among people with work-related injury, the top one occupational category for these who were Hispanics was construction/extraction occupation (22.7%) follow by precision production, craft, and repair (20.2%) and handlers, equip cleaners, helpers, and laborers (16.8%). While transportation and material moving occupations ranked first in people who were non-Hispanic Blacks (26.6%), it ranked third in people who were non-Hispanic Whites (10.5%). There were some other top occupational categories for people with work-related injury who were non-Hispanic Blacks (construction/extraction occupation (9.6%) and install/maintain/repair occupations (9.6%)) and people with work-related injury who were non-Hispanic Whites (services occupation (11.1%) and precision production, craft, and repair (15.4%)).
Conclusion: Racial differences are present in work-related SCI, and the extent of these differences may be explained by English speaking ability. The findings provide a foundation for future research to explore factors that contribute to racial differences in work-related SCI, which could aid in prevention as well as clinical management.
Support: NIDILRR (#90SIMS0016).

