Media contact: Adam Pope, arpope@ub.edu
 Tracie White wants to identify the most common questions and problems patients with new ostomies have during this time to help patients and families improve quality of life in this new reality.University of Alabama at Birmingham School of Nursing instructor Tracie White, MSN, has embarked on a study using telehealth to improve quality of life for patients who require an ostomy after surgery for certain disease processes.
Tracie White wants to identify the most common questions and problems patients with new ostomies have during this time to help patients and families improve quality of life in this new reality.University of Alabama at Birmingham School of Nursing instructor Tracie White, MSN, has embarked on a study using telehealth to improve quality of life for patients who require an ostomy after surgery for certain disease processes.
An ostomy is a surgically created opening in the body for the discharge of wastes often necessary following procedures for conditions such as colorectal cancer, Crohn’s disease or ulcerative colitis. Patients often experience complications with their ostomy, compounding the physical pain, uncertainty and mental anguish already associated with their primary diagnosis.
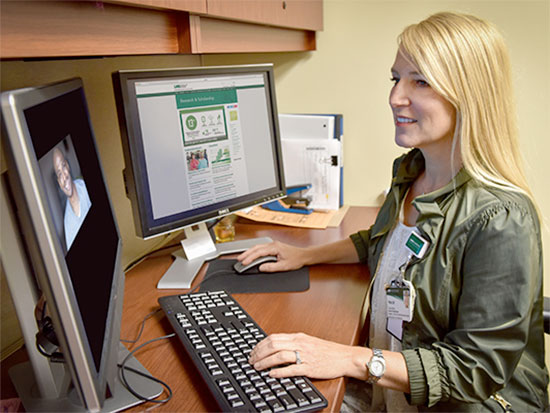
For her study, White is incorporating computer-based, video-sharing software to conduct electronic postoperative visits with patients during the critical time between hospital discharge and scheduled clinic follow-up.
Using the HIPAA-compliant and UAB-approved videoconferencing software RealPresence Desktop, White will visit online with her patients two days after and again one week after hospital discharge.
“Patients typically have about a three-week period before they come back to the clinic for a follow-up visit,” White said. “During those three weeks, problems with their ostomies may result in unscheduled visits to the clinic or emergency room. Being able to see these patients and address their concerns without making them drive back to the hospital increases access to care and provides support during this transition period.”
White wants to identify the most common questions and problems patients with new ostomies have during this time to help patients and families improve quality of life in this new reality. For example, she wants to know whether the ostomy bag is working correctly and whether they and their families are comfortable using it. As a way to revise and improve the process to ensure positive future impacts for patients, she also wants to find out how her current patients feel about using a virtual format as part of their discharge plan. Most of all, she wants to reassure them by addressing concerns face to face.
“Many times, patients struggle because they are embarrassed to call or don’t know whom to reach out to,” White said. “Meeting with them two days after they leave the hospital gives them time to get settled at home and figure out what issues are most important to them. Then, after a week, we can discuss strategies to cope with their new situation.”
White, who earned her Master of Science in Nursing degree as an acute care nurse practitioner from the school in 2010, is collaborating with UAB Hospital’s Division of Gastrointestinal Surgery as part of her faculty practice to work with ostomy patients as part of a project in the school’s Doctor of Nursing Practice program, in which she is a student. In her faculty practice, White collaborates with UAB School of Medicine Dean Selwyn Vickers, M.D., her clinical mentor, Melanie S. Morris, M.D., and other surgeons in the Division of Gastrointestinal Surgery whose patients will make up her study group.
“I hope that knowing they already have a visit with me set up for 48 hours after they are discharged will ease some of their anxiety,” White said. “I want them to look forward to that visit and to talking with me about any issues.”