In our comprehensive one-year advanced heart failure and transplant cardiology fellowship program, you will gain robust comprehensive inpatient and outpatient training in the specialty of heart failure with dedicated educational experience in a multidisciplinary environment.

Fellowship Experience
Thank you for your interest in the UAB advanced heart failure and transplant cardiology fellowship program. We are very proud of our training program as it provides the foundation of excellence for our clinical programs. This fellowship is offered to those who have completed a general cardiology fellowship (PGY7 level or greater) and are seeking advanced training in the subspecialty of advanced heart failure, cardiac transplantation, mechanical circulatory support and pulmonary vascular disease.
Our program highlights include access to our dedicated 20-bed Heart Transplant ICU (HTICU), extensive exposure in dual organ transplant including Heart/Lung & Heart/Kidney combined transplant, robust pulmonary hypertension experience with one of the largest PH clinics in the southeast, and experience in our dedicated ECMO program.
Our program provides superior cardiology training in a collaborative environment. We have specialty clinics across our medical campus, which is anchored by our 1,200 bed inpatient center UAB Hospital—the eighth largest public hospital in the nation. The hospital is in close proximity to the Birmingham VA Medical Center, UAB Hospital Highlands campus, The Kirklin Clinic, and Children's Hospital of Alabama where fellows also train.
Clinical Rotations
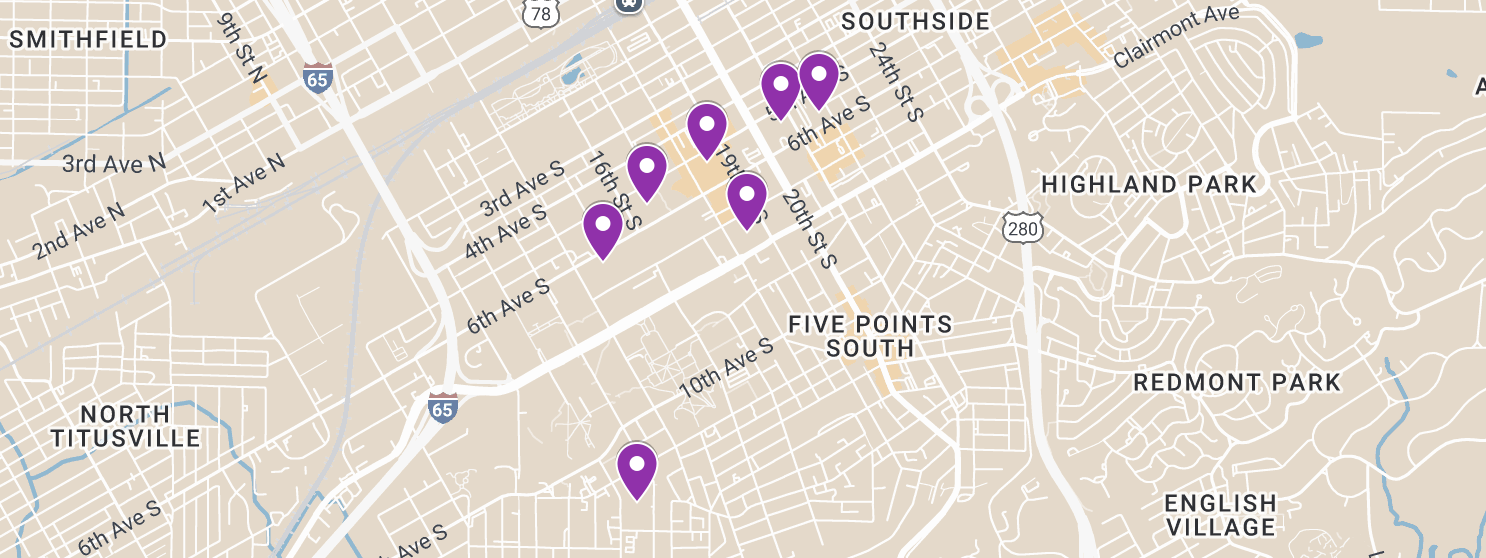 UAB is a highly walkable campus, making it easy to navigate your clinical rotations. Many of our clinical training sites are connected by skybridges, offering protection from rain, heat, and traffic. Browse these buildings to learn more about the types of training conducted there.
UAB is a highly walkable campus, making it easy to navigate your clinical rotations. Many of our clinical training sites are connected by skybridges, offering protection from rain, heat, and traffic. Browse these buildings to learn more about the types of training conducted there.
Explore our training sitesOpens an external link.
Our program offers comprehensive, multidisciplinary training within a collaborative environment. We focus on developing our heart failure fellows by expanding their expertise in areas of advanced heart failure, transplant cardiology, mechanical circulatory support, and pulmonary vascular disease through a combination of inpatient and outpatient care.
At the Kirklin Clinic, fellows will engage in specialized clinics for congestive heart failure, pulmonary hypertension, ventricular assistant devices, transplant, and biopsy suites. At the Birmingham VA Medical Center, fellows manage a panel of patients longitudinally throughout their training. They also participate in Block model rotations, covering general cardiology, arrhythmia, heart failure, pulmonary hypertension, and elective time including adult congenital heart disease.
Our inpatient services are anchored in our heart transplant ICU, where leading-edge clinical programs for heart transplant, VAD, and PH are managed. Our teams work closely with cardiovascular surgery and interventional/structural cardiologist to address cardiogenic shock using temporary MCS techniques like ECMO, Impella, and TandemHeart. Furthermore, we provide exposure to unique clinical programs such as Cardio-Obstetrics, Cardio-Oncology, and Amyloid/infiltrative cardiomyopathies. Our heart failure fellows aid in supporting our team in managing complex valvular diseases.
Research Opportunities
Our program works closely with the UAB Comprehensive Cardiovascular Center to foster multi-disciplinary and multi-investigator collaborations and programmatic development in cardiovascular research. We strive to enrich our fellows training experience by exposing them to cutting-edge research in basic, clinical, population, and translational cardiovascular science.
Let's get acquainted
It's not just what you learn. It's also about the people you learn with. Our cardiology fellowship program leaders are dedicated to developing the potential of every talented trainee.
Meet our people
Frequently Asked Questions
-
What will I need to apply?
All applications are reviewed via Electronic Residency Application Service® (ERAS), #1007152S0. The following documents are required:
-
Current CV (updated within 3 months)
-
Medical School Transcripts (and diploma if requested)
-
Medical School Dean’s Letter
-
Three (3) total Letters of Recommendation (including former program directors)
-
Certificate/verification from previous residency training
-
Must be eligible for Alabama Medical License and Alabama Controlled Substance Certificate (all step scores completed at the time of application)
-
Must be eligible for Federal DEA registration
-
Valid ECFMG Certificate (IMG only)
We do not accept any addtional documents outside of ERAS submissions.
-
-
Are there work requirements to train at the VA?
UAB fellowship programs are fortunate to partner with the Birmingham Veterans Affairs Health Care System as a part of our training experience.
Am I Eligible Checklist: Please ensure that you meet the eligibility requirements for training at the VA by accessing the “Am I Eligible Checklist.” Failure to be able to rotate at a major teaching location will, in most cases, result in a revocation of an offer to train, termination, or non-renewal of your GME Agreement.
Selective Service Registration: VA policy states that any male U.S. citizen who did not register for selective service before age 26 is not eligible to work at a VA, no exceptions. You can register for selective service or verify that you have already registered for selective service online with the U.S. Selective Service System.
-
What are the salaries & benefits for fellows?
Our program provides benefits and insurance plans available to all fellows at UAB. You can find the list of salaries and benefits for fellows based on PGY level here.
-
What is the cost of living in Birmingham?
Birmingham offers a vibrant urban lifestyle at a cost that’s approximately 9% below the national average. Trainees enjoy access to thriving neighborhoods, a nationally recognized food scene, and a dynamic creative community.
-
What are the current vaccination requirements?
Vaccinations are required based on CDC recommendations for Health Care Workers including routine childhood vaccines, Hepatitis-B, COVID-19 and Influenza, except in the case of an approved exemption.
-
Is there a minimum USMLE score required?
There is no minimum USMLE score requirement. We take the score into account as part of the overall review of an application.
-
What are the key program dates for Applications
Applications Open and Close — July through September: Apply through ERAS
Applications Reviewed — August
Interview Invitations Released — August
Interviews Begin — September
Match Day — November
Fellowship begins — July 1
-
Do you sponsor H1B or J1 Visas?
Yes, the division can sponsor these Visas.
Got more questions? Reach out and let's talk.
 It would be my pleasure to speak with you about the amazing training opportunties we provide at UAB. Please contact me if you have any questions about our Advanced Heart Failure and Transplant Cardiology Fellowship.
It would be my pleasure to speak with you about the amazing training opportunties we provide at UAB. Please contact me if you have any questions about our Advanced Heart Failure and Transplant Cardiology Fellowship.
Andrew Lenneman, M.D., Program Director
Send an Email
 I'd be delighted to talk with you about the many exciting possibilities that await you at UAB and Birmingham. Contact me for more details about our heart failure fellowship.
I'd be delighted to talk with you about the many exciting possibilities that await you at UAB and Birmingham. Contact me for more details about our heart failure fellowship.
Joanna Joly, M.D., Associate Program Director
Send an Email
 I'm happy to answer any questions you may have about our exciting program. Please feel free to contact me.
I'm happy to answer any questions you may have about our exciting program. Please feel free to contact me.
Angela Fielder, Education Administrator
Send an Email