2002 Case #1 |
 |
|
| The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. In 2001 we disseminated each week by e-mail an interesting case seen by the course participants that week. Each case included a brief history and an attached digital image pertinent to the case. The diagnosis and a brief discussion were posted at the same time on this website. These are the 11 cases that were presented in that format.
These cases are now available for online CME credit. Please visit UAB CME for more information. |
| The following case was seen on the Medicine Service of Cayetano Heredia Hospital in Lima by the 2002 Gorgas Course participants. |
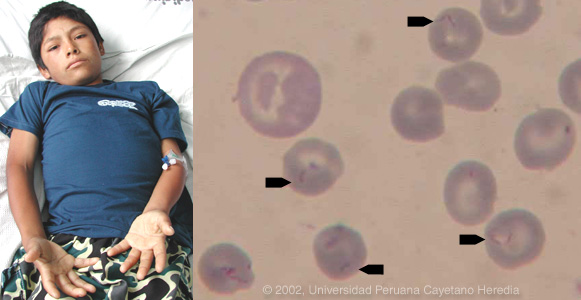 |
| History: 14 yo male presents with 2 weeks of nausea, severe anorexia, fatigue, and noticeable pallor. Afebrile until 5 days prior to admission when onset of fever to 40°C, vomiting, headache and dark urine. |
| Epidemiology: Lives at 3700 meters (12,000 feet) in rural Andes in Ancash Department. Regular trips to nearby valley at less than 3000 meters to buy and sell produce. Was there overnight once during December. |
| Physical Examination: T 38.4°C HR 110 RR 22. Acutely ill and pale but non-icteric. Mild cervical adenopathy bilaterally. No hepatosplenomegaly or lymphadenopathy. Functional murmur with otherwise normal cardiac exam. |
| Labs/X-ray: Hct 16 with with anisocytosis, poikilocytosis, and a 6.8% reticulocytosis. WBC 10.6 with 68 segs, 9 bands, and 21 lymphs. Platelets 105,000. Normal bilirubin and liver function. Normal renal function and urinalysis. A malaria smear was ordered. |
2002 Case #1
|
 |
|
| (Links to Other 2002 Cases are at bottom of this page) | ||
| Diagnosis: The acute form of bartonellosis due to Bartonella bacilliformis. Also known as Oroya fever and Carrion's Disease. |
| Discussion: The blood film showed no malaria but overall 60-70% of the red blood cells contained small pleomorphic coccobacilli intracellularly which are diagnostic of acute bartonellosis. Blood cultures using Ruiz-Casteñeda medium or Columbia agar must be incubated at 25-28°C and take up to 2-4 weeks to become positive. Western blot and PCR are most useful for diagnosis of the chronic eruptive form of the disease (see below) where blood films are usually negative but generally unnecessary in the acute form where, on average, over 60% of erythrocytes have intracellular bacteria.
Clinically the acute phase of infection follows an average 17-day incubation period. Almost all patients have fever, malaise, and anorexia. Pallor is usually noticeable, in hospitalized cases anyway, as the average admission hematocrit is 17%. The anemia is due to red-cell lysis and not autoimmune in nature as the Coombs test is uniformly negative. Hepatomegaly, lymphadenopathy, and jaundice each occur in about 3/4 of cases but splenomegaly in only about 1/4. A significant number of patients may develop congestive heart failure, pericardial effusion, or anasarca, however, an echocardiogram (routinely performed in all patients) was normal in our patient. Neurologic complications of uncertain etiology occur in about 20%; manifestations include altered mental status, ataxia, agitation, or even coma. Our patient had one episode of headache with some mental status changes that lasted for 1-2 days. A secondary immunosuppression may lead to subsequent or concomitant salmonellosis (both S. typhi and non typhi), toxoplasma reactivation and occasionally other opportunistic infections have been seen. In those untreated patients that have unapparent acute phases or survive the primary infection, a chronic eruptive phase occurs. Skin lesions are most commonly miliary in nature with multiple 1-4 mm papular, erythematous round lesions that are often pruritic. These are loaded with bacteria and are histologically similar to HIV related bacillary angiomatosis lesions caused by the related organisms B. henselae and B. quintana. Bartonella henselae is also the agent of cat-scratch disease. The distribution of Bartonella bacilliformis, which is transmitted by the bite of the Lutzomyia verrucarum sandfly is restricted to the inter-Andean valleys of Perú and Ecuador. Classically, transmission was thought to be restricted to 500-2500 meters elevation and between 2-13 degrees latitude in these 2 countries, but more recently cases have been described up to 3200 meters. Of importance to travel medicine physicians, a new focus has been described in the last 4 years in the Urubamba Valley of Perú. So far this focus has not impinged on the portion of that valley traversed by visitors to Machu Picchu, one of the major tourist destinations in South America. Travelers are more likely to encounter bartonellosis when trekking out of Huaraz in the Cordillera Blanca region of the country. In vitro, B. bacilliformis is sensitive to most antibiotics including penicillins (including Penicillin G and ampicillin), cephalosporins, aminoglycosides, chloramphenicol, macrolides, tetracyclines, and quinolones. In the past chloramphenicol has been used extensively in Perú because of its ability to simultaneously cover concomitant opportunistic salmonellosis. Because of increasing salmonella resistance to chloramphenicol and toxicity concerns with this drug, Ciprofloxacin 500 mg po bid for 10 days is now the first line therapy, although clearly almost any available antibacterial agent will suffice for the bartonellosis itself. The present patient received 2 units of packed red cells on admission and has responded well to oral ciprofloxacin. The bartonella and malaria endemic areas of Perú have little overlap. In a traveler to Perú with fever and anemia, the first diagnosis is malaria if they have been to low lying jungle regions but the first diagnosis should be bartonellosis if travel has been restricted to inter-Andean valleys. Untreated bartonellosis will almost always be fatal in a traveler. Antimalarials are not effective against bartonellosis. Always rule out malaria in a tropical traveler to endemic areas but it is important not to let a patient with possible bartonellosis die for lack of a little ciprofloxacin or penicillin. Reference: Maguina C., et al. Bartonellosis (Carrion's Disease) in the Modern Era. Clin Infect Dis 2001;33: 772-9.
|