| 2003 Case #7 |  |
|
| 2003 Case #7 Diagnosis& Discussion |
 |
|
| (Links to Other 2003 Cases are at bottom of this page) | ||
| Diagnosis: Paracoccidioidomycosis due to infection with Paracoccidioides brasiliensis. |
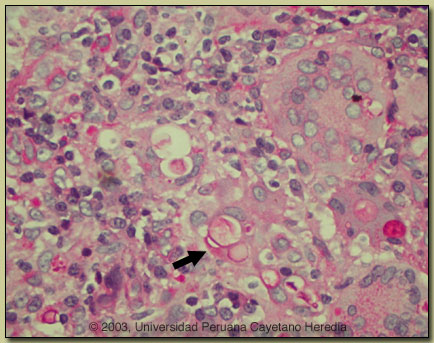 Discussion: The diagnosis was made by simple KOH preparation of a syringe aspirate of a cervical lymph node, which showed typical pilot-wheel shaped organisms consisting of spherical cells 10-40 microns in diameter with a thick birefrigent cell wall surrounded by several peripheral buds. A repeat lymph node biopsy showed granulomas with giant cells, and PAS staining [see image at right] showed characteristic large budding yeast forms of Paracoccidioides brasiliensis. The arrow points to a multiply budding yeast form within a giant cell stained red with PAS. Some singly budding forms can be seen in P. brasiliensis infected tissue. Hyphal forms are not seen in tissue in paracoccidioidomycosis. Culture is pending. A scraping of a forehead lesion was also positive by direct KOH examination. Direct scrapings or aspirates will be positive in the vast majority of cases of paracoccidioidomycosis with mucosal or cutaneous lesions. Discussion: The diagnosis was made by simple KOH preparation of a syringe aspirate of a cervical lymph node, which showed typical pilot-wheel shaped organisms consisting of spherical cells 10-40 microns in diameter with a thick birefrigent cell wall surrounded by several peripheral buds. A repeat lymph node biopsy showed granulomas with giant cells, and PAS staining [see image at right] showed characteristic large budding yeast forms of Paracoccidioides brasiliensis. The arrow points to a multiply budding yeast form within a giant cell stained red with PAS. Some singly budding forms can be seen in P. brasiliensis infected tissue. Hyphal forms are not seen in tissue in paracoccidioidomycosis. Culture is pending. A scraping of a forehead lesion was also positive by direct KOH examination. Direct scrapings or aspirates will be positive in the vast majority of cases of paracoccidioidomycosis with mucosal or cutaneous lesions.
Paracoccidioidomycosis is most often an indolent and relapsing disease even in the face of adequate therapy and normal host immune status. Primary pulmonary infection may be asymptomatic and self-limited but even with treatment will produce at least moderate pulmonary fibrosis. This patient presents an example of the chronic progressive disseminated form of the disease. The chest x-ray shows some atelectasis with some patchy areas of interstitial fibrosis; this is compatible with fibrotic scarring or residua from more active pulmonary disease in the past. At the outset of progressive pulmonary disease, scattered areas of both interstitial and alveolar consolidation are seen, often bilaterally and usually in the middle and lower zones of the lungs. With progressive fibrosis coalescent nodules may form. A miliary pattern may been seen in acute disseminated disease. Paracoccidioidomycosis, also known as South American blastomycosis is found in humid forested or lush green areas of the Americas from Southern Mexico south to Uruguay and Argentina. It appears to be most common in Brazil. The exact habitat of the organism is unclear but transmission is described as being entirely by airborne inhalation. However, we have observed cases with only oral lesions apparently associated with the use of tree leaves contaminated with fungal spores as toothpicks. Similarly the use of leaves as toilet paper has resulted in anal infections that can be confused with anal cancer. Rural adult males agricultural workers between 30-60 years of age are most affected by the infection. Travelers spending less than 6 months in an endemic area are unlikely to acquire paracoccidioidomycosis. Extrapulmonary disease is found in over 70% of cases and may involve mucous membranes most frequently (painful oral lesions that may be confused with mucocutaneous leishmaniasis), skin (usually facial areas), lymph nodes, adrenals, abdominal organs and CNS (in 10%). 15% of our patients have concomitant pulmonary TB. In known endemic areas a combination of radiologic findings with characteristic oral, cutaneous, or osseous lesions are highly suggestive of the diagnosis. However, in many co-endemic areas it is often difficult on clinical grounds to distinguish isolated pulmonary disease due to paracoccidioidomycosis from tuberculosis or from other deep mycotic infections such as histoplasmosis. Sulfonamides, ketoconazole, itraconazole, and amphotericin B are all effective therapies. Amphotericin should be reserved for severe cases. While itraconazole 100 mg/day for 6 months or so is regarded as the treatment of choice, in the developing world setting ketoconazole is likely equally effective and is usually less than half the cost. However, at least 12 months of therapy with ketoconazole is generally recommended. Paracoccidioidomycosis is always a severe infection that may relapse even after prolonged treatment, so it always needs to be treated and followed up aggressively.
|
