 |
Gorgas Case 2005-03 |
 |
|
This past week the Gorgas Expert Course concluded and the Gorgas Diploma course commenced. The following patient was seen by course participants in the outpatient department of the Tropical Medicine Institute. We wish to acknowledge the advice of Dr. Betty Bustamente, Director of Mycology at the Tropical Medicine Institute and of Dr. Juan Carlos Ferrufino of the Pathology Department, UPCH.

 History: 29 year-old male with a 17-year history of an indolent proliferative lesion on the left ear. Initially the lesion was a pruritic papule, then multiple papules but has increased greatly in the past 4 years. Initially, he was treated for cutaneous tuberculosis and then leishmaniasis despite lack of histological proof, with no improvement either time. Multiple subsequent biopsies have been inconclusive. No other local or systemic symptoms.
Epidemiology: Forestry worker from Madre de Dios (Tambopata/Manu Park) in the low jungle of southern Perú who has lived most of his life in forested areas of the region. Has traveled to Brazil but after onset of lesions. Physical Examination: Afebrile. No lymphadenopathy. Abnormalities restricted to the proliferative keloidal lesion shown in Images A and B. No discharge or purulence. Oral cavity normal. ENT otherwise normal. Laboratory Examination: Hb 14.7. WBC 6.1 with 60 segs, 29 lymphs, 3 monos, 3 eos. Biochemistry unremarkable. Chest x-ray normal.
|
|
Diagnosis: Lobomycosis due to Lacazia loboi (formerly Loboa loboi). Sometimes referred to as Lobo's Disease or as keloidal blastomycosis.
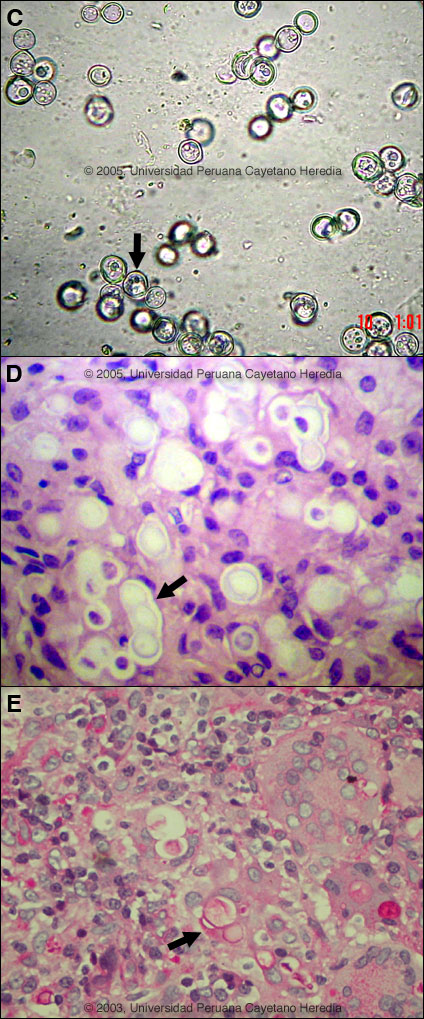
 Discussion:Lacazia loboi cannot be cultured and all fungal cultures as expected were negative. A direct KOH prep [Image C] was consistent with the diagnosis containing abundant refractile globose 9 µm cells with blastoconidia sometimes appearing in chains. Short tube-like connectors are seen between organisms [arrow]. A biopsy [Image D] demonstrates characteristically refractile cells producing blastoconidia with all cells being of equal size [cf Paracoccidioides in Image E where blastoconidia are of different sizes]. Some organisms are found in chains [arrow, Image D] as is almost always seen with Lacazia but not Paracoccidioides. An inflammatory infiltrate of histiocytes is present and in some patients, the dermis may be completely replaced by histiocytic granuloma. Stains of the biopsy for AFB and leishmania were negative. Differential diagnosis of this lesion includes subcutaneous mycoses (chromomycosis, sporotrichosis, eumycetoma), cutaneous tuberculosis, leprosy, leishmaniasis, and benign and malignant tumors (e.g., Kaposi's and other sarcomas). Lobomycosis is characterized by a chronic, painless very slowly progressive granulomatous infection of skin and subcutaneous tissue with no contiguous invasion or systemic spread. Lesions are usually asymmetrical and keloidal often beginning as nodules. Verrucous and ulcerative forms may also occur. Lesions are most often on the leg, followed by the ear. Lesion durations of over 50 years have been documented. First described in 1931 in Brazil by Jorge Lobo, it was thought to be a manifestation of paracoccidioidomycosis. Indeed, recent DNA analysis [J Clin Microbiol 1999 Jun;37(6):2031-3] has confirmed a close relationship to P. brasiliensis. Approximately 500 cases have been reported mainly from Brazil and Surinam, but also from French Guiana, Colombia, Venezuela, Ecuador, Bolivia, Mexico and Perú. This is only the second case seen at our institute, the initial case presenting with a leg lesion. Infections also occur in dolphins off the coast of Florida, Surinam, and Brazil but the normal ecologic characteristics of Lacazia loboi are unknown. The only know effective treatment is surgical excision. Ketoconazole is clearly ineffective. Given the location of the present lesion definitive excisional surgery is not feasible. Given the known responsiveness of blastomycosis and paracoccidioidomycosis to itraconazole the patient has been given a trial of therapy with posaconazole on a compassionate use basis, courtesy of Schering-Plough. Response after 3 months of therapy has been modest.
|