| 2005 Case #6 |  |
|
| Diagnosis: Furuncular myiasis due to Dermatobia hominis. Also called the human botfly. |
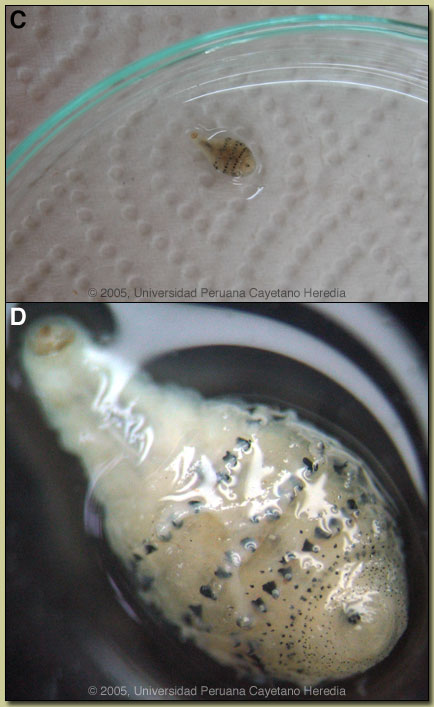 Discussion: The patient declined an offer of surgical excision while in clinic. Upon return home, on the advice of a friend, the patient applied occlusive therapy with some tobacco and 4 hours later the botfly larvae began to emerge and was then fully pulled out by the patient. The larva is shown in Images C & D. The broad end with the black respiratory spiracle is of necessity always located closest to the surface thus making removal more difficult. Discussion: The patient declined an offer of surgical excision while in clinic. Upon return home, on the advice of a friend, the patient applied occlusive therapy with some tobacco and 4 hours later the botfly larvae began to emerge and was then fully pulled out by the patient. The larva is shown in Images C & D. The broad end with the black respiratory spiracle is of necessity always located closest to the surface thus making removal more difficult.
Myiasis is defined as the infestation of humans or other vertebrates with larvae (maggots) of Diptera (or true flies), with the larvae feeding on the host?s living or necrotic tissue. In primary myiasis, the larvae themselves burrow into intact skin and secondary myiasis is due to larval deposition into devitalized or necrotic tissue such as in wounds. The families of Diptera causing various forms of myiasis are very diverse and many have specific geographic distributions. In furuncular myiasis the larvae penetrate intact living skin but cannot penetrate beyond the subcutaneous tissue developing into an expanding boil-like lesion. In the tropical Americas, furuncular myiasis is due to Dermatobia hominis, the human botfly. The adult female fly physically captures a mosquito and then glues her eggs to the abdomen of the carrier mosquito. When the mosquite next feeds on a human or animal the eggs drop off, hatch and a larvae inside burrows through the skin. Botfly lesions are almost always single, and the point of the furuncle is characterized by a small punctum through which the larva must obtain oxygen [see Image B]. Occlusion of the respiratory punctum such as with paraffin or petroleum jelly often causes the pear-shaped larva to come out and is curative. Surgical excision under local anesthesia is necessary for refractory cases. Professor Hugo Lumbreras, the founder of our Tropical Medicine Institute, used to teach of the traditional approach to myiasis in Peru, which involved the occlusion of the entrance of the wound by a solution made from basil leaves, the odor of which forced the larvae out of the wound. Bacterial superinfection of Dermatobia hominis furuncles may sometimes occur. In Africa, furuncular myiasis is caused by Cordylobia anthropophaga or Tumbu fly (not to be confused with tungiasis caused by the sand flea Tunga penetrans). The Tumbu fly directly lays her eggs on dirty or soiled clothing. If not properly washed and ironed (heat kills the larvae) the eggs hatch and invade skin when the clothing is next worn. Lesions are almost always numerous and tend to be angrier and more erythematous than with the botfly. Bacterial superinfection is extremely uncommon with Cordylobia anthropophaga.
|
