 |
Gorgas Case 2007-06 |
 |
|
The following patient was seen in the inpatient department of the 36-bed Tropical Disease Unit at Cayetano Heredia National Hospital.
History: 57-yo male who noted a papular and erythematous lesion on the nose fourth months ago that was not associated with pain, itching or constitutional symptoms. Two months ago he noticed a single episode of epistaxis, and progressive enlargement of the lesion with infiltration of the nasal mucosa of the left side that produced nasal obstruction and anosmia. Two weeks before admission the patient noticed severe constant headache and presented for further evaluation. Itraconzale (100 mg/d) and co-trimoxazole were started 2 months earlier at another hospital with minor improvement of the skin lesion. He has been previously healthy with no history of sinus, nasal, or neurologic problems. Epidemiology: The patient is a farmer from Sechura, Piura in the coastal desert 900 km north of Lima. He raises cattle, cats, and dogs, and he fishes and collects bamboo in local rivers and ponds. No known exposures to TB, ill people, or ill animals. Physical Examination: Afebrile. Infiltrative and erythematous lesion on the nose [Image A]. Nasal mucosa with an edematous and erythematous mucosa and deviation of the septum to the left. The rest of the exam was normal including a complete neurologic exam. Laboratory Tests: Hematocrit 40%, WBC 14,000 (78% neutrophils, no eosinophils), platelets 480,000. Normal liver function and chemistry. Cerebrospinal fluid with 364 white cells, 62% polymorphonuclear cells, 38 mononuclears; glucose 45 mg/dl (normal), proteins 95 mg/dl (high); gram stain negative, India ink negative and bacterial culture negative. HIV negative. MRI shows multiple enhancing lesions located in the cerebral parenchyma, cerebellum and brainstem [Images B and C]. Involvement of the right frontal sinus and extensive involvement of the nasal mucosa of both sides but specially the left side is also observed [Image D]. A biopsy was obtained. 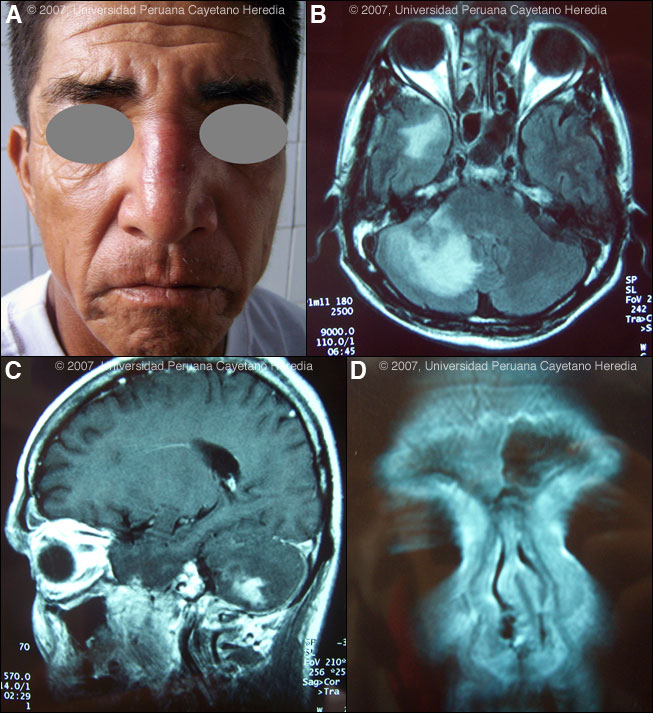
 |
|
Diagnosis: Balamuthia mandrillaris (free-living amoeba).
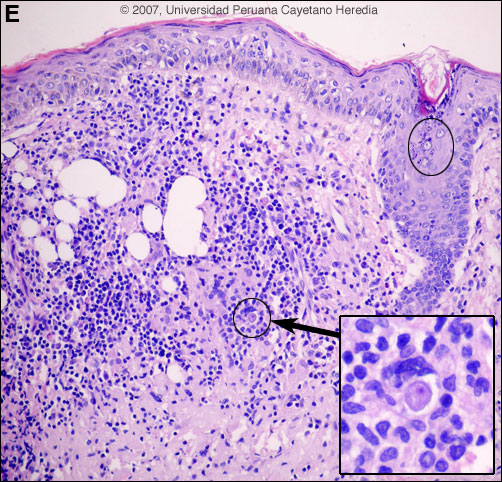
 Discussion: A skin biopsy of the lesion over the nose showed a dense immflamatory infiltrate of the dermis composed of lymphocytes, plasma cells and multinucleated cells with granulomas. There are multiple trophozoites of a free-living amoeba [Image E, ovals]. Note the small nucleus eccentrically located and the vacuolated cytoplasm [Image E, magnification]. Definitive identification of Balamuthia requires culture or specific immunostaining, and successful use of PCR has been reported. However, other species of free-living amoeba are not known to occur in Perú. Around 100 cases of Balamuthia mandrillaris have been reported since the organism’s initial description in 1990 [Clin Infect Dis. 1997 Dec;25(6):1354-8]. Half or so have been in the USA, mostly in immunocompromised patients. Cases have also occurred in Canada, Mexico, Australia, Argentina, Brazil, Mexico, Thailand, Japan, the Czech Republic, Portugal, and England. A significant number of the published cases from the United States have occurred in persons of Hispanic ethnicity. Additional reports have come from Canada, Japan, Australia, Thailand, and Eastern Europe, as well as from throughout Latin America. We have seen over 50 cases at our institution and, like most Latin American cases, the patient is not immunocompromised. Unlike Acanthamoeba and Naegleria species, which are more familiar to clinicians and known to occur in brackish ponds and creeks, an ecologic niche in nature has not been definitively found for Balamuthia. Our patients have come from throughout rural areas of Perú, and usually, but not always, have a history of swimming in potentially contaminated fresh water. Entry of water into the nasal mucosa and the olfactory nerve endings is thought to occur with Acanthamoeba and Naegleria. Naegleria infection causes an acute necrotizing and suppurative meningoencephalitis, an aggressive disease that is generally fatal in days. Acanthamoeba cause a sub-acute granulomatis encephalitis with a more prolonged but ultimately fatal course. Occasionally patients with Acanthamoeba have a skin lesion usually described as a chronic ulcer. Acanthamoeba, unlike Balamuthia, has been associated also with amoebic keratitis, a painful sight-threatening disease of the eye. In Balamuthia infection the disease may follow a prolonged course, but most frequently has a fatal outcome. Almost all cases have an initial skin lesion, and this lesion precedes the inevitable CNS disease (granulomatous amebic encephalitis) by weeks or months. Patients have ranged from 5 to 65 years of age with 50% under age 15. The typical skin lesion is a single painless plaque up to several centimeters in diameter; a few patients have had 2 to 3 lesions. Color may be skin tone, dark red, or slightly violaceous. Sensation is preserved. Location is usually on the central face but occasionally on trunk or extremities. For facial lesions the differential diagnosis may include tuberculosis, mucocutaneous leishmaniasis, leprosy, sporotrichosis, paracoccidioidomycosis, rhinoscleroma, or mucormycosis. Sarcoid, discoid lupus, and Wegener's can also be considered. Histologically, granulomatous inflammation with lymphocytes, histiocytes, plasma cells, as well as giant cells, is characteristic. Amoebic trophozoites are often scanty and multiple sections need to be examined. Some foci of vasculitis may be present. CNS involvement manifests with heachache, photophobia, seizures that progress to lethargy, sensorimotor deficit, coma and death. The CNS lesion is a progressive hemorrhagic necrosis with large numbers of amoebic trophozoites and cysts invading vascular sub-adventitial areas of arteries, veins, and capillaries, leading to perivasculitis and cerebral infarcts [Hum Pathol. 1999 Mar;30(3):269-73]. No therapy has been shown to be highly effective in curing Balamuthia infection. With IV amphotericin B or pentamidine, an initial and apparently favorable response or disappearance of cutaneous lesions still does not halt the eventual appearance of CNS disease. Similarly, in our hands, multi-drug combination therapy with agents such as albendazole, itraconazole, or fluconazole have still resulted in eventual appearance or progression of CNS disease. In our hands there have been 4 survivors out of 10 patients treated with aggressive combination therapy followed by 6-12 months of albendazole maintenance. One or two case reports from other centers have reported success with regimens that have also included sulfadiazine, macrolides and phenothiazines. The current patient was started on fluconazole 400 mg/d, albendazole (800 mg/d) and amphotericin B 1.0 mg/kg/d. He developed gait abnormalities and increased intracranial pressure on Day 3 of hospitalization and died 1 week later.
|