 |
Gorgas Case 2022-01 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are usually given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Peru. This year, due to the pandemic, we have decided to continue offering the Course, now in its 27th edition, using a mixed educational model involving a virtual format followed by a live session at the Tropical Medicine Institute. New cases will be published every two weeks for the duration of the course. Each case includes a brief history and digital images pertinent to the case. A link to the actual diagnosis and a brief discussion follows. Carlos Seas and German Henostroza |
|
The following patient was seen in a private clinic in Lambayeque.
 History: A 43-year-old male with a history of laryngeal carcinoma was treated with total laryngectomy and tracheostomy two years ago. He presented to his oncologist complaining of two weeks of purulent secretion through the stoma and the presence of “worms” crawling in the stoma. He denied fever and other constitutional symptoms. Epidemiology: The patient lives in a rural area of Northern Peru. He is a farmer and has regular contact with cattle, goats, guinea pigs and dogs. The remainder of his past medical history was unremarkable. Physical Examination: The tracheostomy was found to have significant erythema. Several small white organisms were removed [see Video A]. Laboratory: Hb: 14.5 g/dL; Hct: 42%; WBC: 4,500 (Neu: 55%, Eos: 1%, Lymphs: 35%, Monos: 7%, Bas: 2%); Platelets: 240,000; Gluc: 84 mg/dL; Urea: 18 mg/dL; Creat: 0.9 mg/dL.
|
|
Diagnosis: New world screwworm due to Cochliomyia hominivorax. 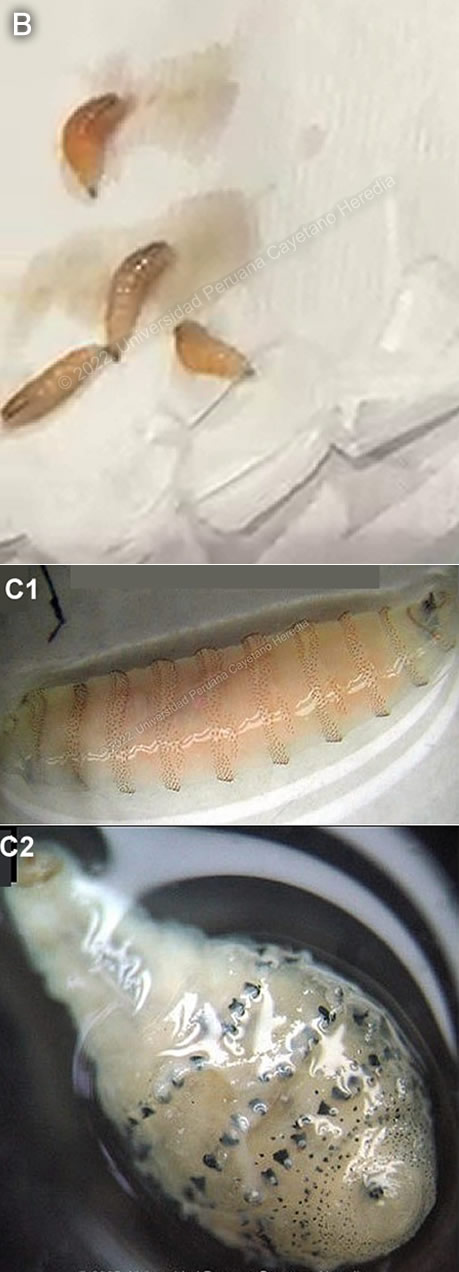
 Discussion: Approximately 10 live maggots were extracted from the site of infection [Image B]. The patient immediately underwent surgery, where more than 30 additional maggots were extracted. The maggots were found to be fourth-stage Cochliomyia hominivorax. Cochliomyia larvae typically have a smooth external aspect, with dorsal tracheal trunks and are pigmented. Two other distinctive features of the larvae that are difficult to appreciate in the image are the open peritreme, found at the tail, and the posterior spiracles [Image C1]. In contrast, Dermatobia hominis larvae are hairy, pear-shaped, with transverse bands of hooks and a respiratory spiracle in the broad end [Image C2]. Myiasis is the infestation of humans and other vertebrates with the larval stages (maggots) of various flies. Flies in several genera may cause myiasis in humans. Dermatobia hominis is the primary human bot fly. Cochliomyia hominivorax is the primary screwworm fly in the New World and Chrysomya bezziana is the Old-World screwworm. Cordylobia anthropophaga is known as the tumbu fly. Flies in the genera Cuterebra, Oestrus and Wohlfahrtia are animal parasites that also occasionally infect humans. Dermatobia hominis and C. hominovorax are Neotropical species, ranging from Mexico into South America. A recent report from Northern Peru documented that 5 of every 9 cases of myiasis in the region were due to C. hominivorax, and 4 of these 5 had associated cancers [AJTMH]. Another report from Ecuador documented 39 cases of myiasis, wherein 15 were caused by C. hominivorax [PNTD 2019]. Screwworm myiasis is often associated with pre-existing wounds, though infestation can also occur on mucous membranes, such as nostrils, eye orbits, ears, mouth, and genitalia. Nearly any wound is susceptible to screwworm infestation. This includes natural wounds received from arthropod bites, fighting, and disease, or wounds resulting from farm management procedures such as barbed wire fencing, dehorning, castration, and ear tagging. Navels of newborn mammals are also common sites for screwworm infestation. Characteristics of infested wounds include drainage, suppuration, discharge of blood and serum, and distinctive odor. Secondary bacterial infections are also likely to occur. Animals with screwworm infestations often display discomfort, lethargy, and depression, and they may separate from the herd. In humans, the highly invasive screwworm larvae produce deep lesions of 5 cm or more. Their spines are used as anchors, making extraction difficult. Moreover, the odor of the lesions attracts other gravid female flies, which leads to a single wound containing hundreds or thousands of larvae. When mature, the larvae fall from the host to pupate in the soil and develop into adult flies. This cycle typically takes 3 weeks, but may take several months in cooler climates such as that of the Andes. One of the first descriptions of human infestation with screwworm was in 1858 among prisoners of Devil’s Island in French Guiana. Coquerel reported 3 mortalities in 6 of the patients involved, and screwworm was said to have been responsible for hundreds of deaths over the years in Devil’s Island. Interestingly, the name itself, hominivorax, means “man-eater” in Latin. In contrast, botflies and tumbu flies cause a furuncular form of myiasis, with a single boil-like painful lesion in healthy tissue, with a small punctum on top of the furuncle through which the larvae obtain oxygen. Discharge of an exudative material or air bubbles through the small punctum is characteristic and should raise suspicion of furuncular myiasis. Some patients even mention that they feel the larva moving inside the skin. There are no applicable serological tests, nor are they indicated in the identification of this disease. The diagnosis of myiasis is made by identification of the species of the extracted larva. There have been reports of successful treatment of screwworm infestations in Ecuador with the use of ivermectin, either topically or orally for 5 days in addition to manual extraction of the maggots [PNTD 2019]. Oral ivermectin has also been used successfully to treat ocular myiasis due to C. hominivorax, with doses up to 400 ug/kg. Ivermectin paralyzes the maggots and prevents further tissue damage, limiting more extensive debridement [CID 2006]. Programs in the 1970s and 1980s aimed to eradicate new-world screwworm in the United States through the use of sterile male flies, but outbreaks in deer have been reported as recently as 2017 in Florida, requiring new large interventions [J. Med. Entomol.]. Similar campaigns are ongoing in Mexico and Central America. |