-
Beginnings of Pediatric Emergency Medicine in Alabama
Holy Innocents Hospital for Children was founded in 1911 located in the All Saints Parish House. Its name was changed to Children’s Hospital of Birmingham in 1914 and moved to a new building on 30th Street and 7thAvenue South in 1924. Outpatient services were first provided in 1925 but according to pediatrician Dr. Vince Carnaggio, “On 30th Street there really wasn’t an emergency department, you might meet a patient down there and then ask a nurse down from upstairs to help you out. You would see someone who just dropped in. The 30th Street facility would be sort of a source of referrals, but you just saw patients wherever they happened to show up.”
In 1959 the emergency department (ED) was in the “Hole” in the Hillman building, UAB’s first hospital. The Hillman Hospital was where the primarily African American children’s ward was located, though African American children were also provided care at Children’s Hospital. Children’s Hospital and UAB were separate entities until establishing a collaboration agreement when a new facility was opened in 1961, after which the majority of pediatric care was provided at Children’s Hospital, including emergency medicine.
The new facility was located on 6th Avenue South, between 16th and 17th streets. Between 1961 and 1982, the emergency department entrance was on 17th Street.A local pediatrician, Dr. Don Palmer, who started the Greenvale practice, was active in prevention efforts and began taking poison center calls (writing them on index cards) in 1958. The poison center started providing 24/7 access in 1978.
Paul Palmisano, M.D., MPH, arrived at UAB in 1966. Being both a pediatrician and pharmacologist, his focus was on poisoning prevention, as well as injury prevention and child safety in general. He recognized patterns that would cause injury to children and would develop strategies to avoid those injuries. He was known as a superb educator and patient advocate. He became the director of Student Affairs and assistant dean of the Heersink School of Medicine in 1973. His mentorship and passion for injury prevention continues today, the baton passing to Drs. Carden Johnston, Bill King, Michele Nichols and Kathy Monroe.
-
1970s
In 1970, Dr. Warren Derrick, after finishing an infectious disease fellowship with Dr. Hugh Dillon, took over the clinics and stayed on until 1976. He established an acute care “dispo” clinic, which provided episodic unscheduled primary care for minor illnesses. Residents would see patients in the acute care clinic until midnight when it closed and patients would then go to the ED. The acute care clinic consisted of four cubbyholes with curtains and no privacy, in addition to four holding cubicles, which were seldom used due to a lack of staffing. Residents performed all venipunctures and did their own gram stains.
Dr. Carden Johnston was originally hired as a hospitalist in 1974, but took over management of the clinic in 1977. The combined volume in the dispo clinic and ED that year was 20,000, with the large majority being seen in the dispo clinic.
In 1971, Geni Smith, RN, finished nursing school and started working at Children’s Hospital. After three weeks of floor nursing, she was taken to ED by the Director of Nursing, Ms. Petri, who informed Geni she would be running the unit on the 3-11 evening shift. The ED consisted of four rooms. When a patient arrived, following a brief observation, she would have to track down a physician appropriate to the complaint. Because there were no beepers, she would have to call to let a doctor know what was happening so the physician could make a decision about whether to come to see the patient. If a patient presented with an injury, Geni would see the child, take the appropriate x-ray and then call the orthopedic doctor, who would expect an interpretation of the radiograph. Then the orthopedist would come see the patient. Dr. Johnston’s son Robert was injured in a fall and was taken to the ED where Geni saw him, got an x-ray, diagnosed his fractured clavicle, put a figure-8 splint on him and sent him home with no physician involvement. Geni later became the trauma team coordinator and retired in 2017.
-
1980s
From 1978-1983, Dr. Carden Johnston was active lobbying the state to implement laws protecting children, requiring the use of car seats as one example. Dr. Johnston was the American Academy of Pediatrics (AAP) Alabama Chapter chairman from 1980 to 1983, and has represented Alabama on a multitude of national committees of the AAP and became the first Alabama Chapter member to become a national advocate for children as AAP President in 2003. In the early 1990s, he created and starred in an award winning weekly safety news segment educating the public about injury prevention on NBC 13 called KidCheck, which was nationally syndicated and ran for about 10 years. Dr. Johnston retired from clinical work in 2005, but as a professor emeritus continues to be active educating residents and students on child advocacy.
The ED changed location and size as part of a hospital expansion in 1982, moving the entrance from 17th Street over to 6th Avenue South. It went from four beds to eight emergency (medical and surgical) beds with an additional five beds for six-hour holding, and eight beds were referred to as the Acute Medical Clinic (ASM), which essentially moved the dispo clinic to be contiguous to the ED, and was staffed by residents who could consult general pediatrics faculty, Drs. Kathe Nelson and Coralie Hains. Showers for decontamination and negative pressure rooms were added at that time as well. According to Dr. Johnston, there was no sign indicating the ED entrance. Pediatric residents were seeing medical complaints, while the surgical and orthopedic residents were treating injuries. There were no attendings in the emergency department. Residents worked 36 hours taking breaks as they needed. Nurses were not allowed to start IVs, as decreed by Department Chair, Dr. Bill Benton, leaving that task to the residents. Neurosurgical patients would go to University Hospital where neurosurgery was located as there were no pediatric neurosurgeons. Private doctors would come to see their own patients in the ED.
The critical care transport team was started in 1983 but was part of the UAB transport team. It was staffed by moonlighting pediatric residents and the vast majority of pediatric transports were for neonatal patients. The ED and AMC saw 40,000 patients that year. National interest in pediatric emergency medicine was beginning to increase, with section status in the AAP starting in 1981 and the first textbook of pediatric emergency medicine published in 1983 by Steve Ludwig and Gary Fleisher, both at Children’s Hospital of Philadelphia at the time. The interest expanded to the pre-hospital environment the following year when Dr. Cal Sia and Hawaiian Senator Inouye introduced legislation for EMS-C (emergency medical services for children). The initial funding of the program began in 1986 and included a total of $2 million per year for state grants. Alabama and UAB received one of the four grants awarded that year, shared by surgeon Dr. Max Ramenofsky in Mobile, Alabama.
1986 was a big year in the growth of pediatric emergency medicine at UAB. Dr. Johnston was given permission to set up an emergency medical service at Children’s, which included a pediatric emergency medicine fellowship. The trauma center was also started that year with no medical involvement from the ED faculty. This was still before there was an attending present in the emergency department for anything other than consults. The residents ran unit and did not feel the need attendings to be present. The residents had the autonomy and responsibility to manage patients, make decisions and learn. Dr. Jake Vacarella, who completed his pediatric residency at UAB in 1982, joined the faculty in March 1987. He and Dr. Johnston decided to cover the ED from noon until midnight, 365 days a year, with one of them physically present in or near the department for 12 hours every day for over a year. Thanks to Drs. Johnston and Vacarella, who paved the way for us today!
Dr. Sergio Stagno’s appointment as chair of the Department of Pediatrics and physician in chief of the Children’s Hospital became official in 1989. Dr. Rud Polhill left private practice to join the department in 1989 and was appointed by Dr. Stagno as the director of both emergency medicine and general pediatrics. Dr. Polhill was one of the first two pediatric interns at the new Children’s Hospital facility and was chief resident in 1970-1971. He was in private practice for 13 years before joining the faculty. He died at the early age of 60 in 2002 from heart disease. The division continues to mourn his passing and celebrate his life and love of learning. Once a year we sponsor a memorial grand rounds speaker and present the Rud Polhill Award to a pediatric intern and a graduating emergency medicine resident who have demonstrated intellectual curiosity and a love of learning.
-
1990s
The emergency medicine faculty in 1990 included Drs. Johnston, Polhill, Vacarella, Karin McCloskey, who joined the faculty after being the first pediatric emergency medicine fellow at UAB, and Dr. Michele Nichols, who had just completed her pediatric emergency medicine fellowship at Cincinnati Children’s. Dr. McCloskey’s academic interest was critical care transport and she worked with the nurses to set up the transport team. She also advocated, applied for and created a section of transport in the AAP. Health issues forced her departure in 1994 and she died unexpectedly in 2007.
On her arrival, Dr. Nichols quickly became a leader in the division assuming responsibility for fellowship training, resident education and toxicology becoming the poison center medical director. Her compassion, work ethic, passion for teaching and academic focus in toxicology and poison prevention were more than reminiscent of Dr. Paul Palmisano.
Dr. Stagno appointed Dr. Nichols, along with Dr. Ray Watts, the assistant residency directors in 1992 and they assumed the role of co-program directors in 1995. Dr. Watts later stepped down and Dr. Nichols continued (to the present day) as the program director of one of the best pediatric residencies in the country. She continued as our fellowship director from 1991 – 2003, then as the co-director with Dr. Ann Klasner from 2003-2008, after which Dr. Klasner took over the role. Dr. Nichols remains the co-medical director of the Regional Poison Control Center. Dr. Stagno appointed her the vice-chair of Education for the department in 2014.
The American Heart Association (AHA) published the Pediatric Advance Life Support (PALS) course in 1998 which our division has been teaching to residents, physicians and nurses ever since. Dr. Vacarella was one of the first PALS national faculty. Dr. Kathy Monroe assumed administrative responsibility for the course when Dr. Vacarella left. Dr. Monroe handed it off to Dr. Annalise Sorrentino, who joined the faculty in 2003 after completing her pediatric emergency medicine fellowship at UAB. Dr. Sorrentino quickly became established as a leader in pediatric education and continues to be in demand as a speaker regionally, nationally and internationally. She is also active regionally and nationally with the American College of Emergency Physicians. Dr. Sorrentino handed administrative responsibility for the PALS course to Dr. Terri Coco, who joined the faculty in 2005 after completing her pediatric emergency medicine fellowship at UAB. Dr. Coco is the Regional AHA director (no longer have national faculty) and the director of all courses offered at Children’s of Alabama (~16/year). She is also co-director of our fellowship.
Bill King RPh, MPH, DrPH, worked as a pharmacist at Children’s Hospital, taught pharmacology at Samford, joined the UAB faculty in 1991 and further developed the Regional Poison Control Center. He obtained his graduate degree in Epidemiology with a thesis on e-codes (external cause of injury), which enables injury data collection. He created the Southeast Child Safety Institute with the goal of reducing injuries to children and along with Dr. Polhill established and managed the Pediatric Health Information Line (PHIL) in 1996. PHIL uses nurses, who follow Barton Schmitt telephone protocols, to provide advice to parents after their pediatrician’s office has closed. Data showed that PHIL reduced unnecessary use of the ED and appropriately referred patients to the ED who otherwise would have stayed home. Needless to say PHIL was warmly received by area pediatricians, and is still used today. Dr. King, who retired in 2017, provided invaluable epidemiological and statistical support for most of the clinical research conducted in the division.
The first pediatric emergency medicine sub-board certification occurred in 1992. The Division of Pediatric Emergency Medicine was officially established in 1993, and Dr. Stagno appointed Dr. Jake Vacarella as division director effective June 1st. Faculty at that time included:
-
Jake Vacarella, Director
-
Tim Givens – Fellowship: Cincinnati Children’s
-
Bill Hardwick - Fellowship: UAB
-
Carden Johnston
-
Karin McCloskey - Fellowship: UAB
-
Michele Nichols – Fellowship: Cincinnati Children’s
-
Rud Polhill
-
Lisa Santer – Fellowship: Case Western Reserve
Dr. Vacarella decided to return to private practice pediatrics in Wisconsin in 1995 and Dr. Roger Berkow, a member of the Division of Hematology Oncology, was appointed acting division director and chair of the Pediatric Emergency Medicine Division Director Search Committee. At that point Drs. Lisa Santer and Karin McCloskey had left and Dr. Tim Givens moved to Louisville in early 1996 to become their fellowship director. Dr. Monroe joined the faculty after completing her pediatric emergency medicine fellowship at UAB in 1995, leaving a total of only five faculty remaining in the division. Dr. Monroe quickly took on leadership roles in PALS, research, injury /advocacy and the AAP. The ED continued to be resident run with injuries still being seen by surgical resident moonlighters. There was no faculty presence after midnight. More than 50,000 patients were being seen in the ED that year.
Dr. Pete Glaeser, who had practiced pediatric emergency medicine at the Children’s Hospital of Wisconsin/Medical College of Wisconsin for 12 years, was hired as the new division director arriving at UAB in the spring of 1996 (much to the relief of Roger Berkow!). The ED entrance was still on 6th Avenue and there were 20 rooms, including a five bed holding area and a two-bay trauma room. Children’s Hospital signed a contract in October of 1996 with Health Services Foundation (HSF) to provide financial support to enable the hiring of additional pediatric emergency medicine faculty to provide 24/7/365 attending coverage in the ED. Surgical moonlighters were phased out and pediatric residents began learning and performing laceration repair and other injury related procedures. ED attendings and fellows and pediatric residents also assumed additional trauma team roles.
By 1999 PEM Faculty included: (year joined faculty)
-
Steve Baldwin (1996) – Fellowship: in PEM and Critical Care, UAB
-
Jud Barber (1999) – Fellowship: UAB
-
David Bernard (1997) – Fellowship: Johns Hopkins
-
Kim Copeland (1996) – Fellowship: UAB
-
Michelle Embling (1999) - Fellowship: UAB
-
Pete Glaeser- Division Director
-
Bill Hardwick- Fellowship: UAB Carden Johnston
-
Ann Klasner (1998) – Fellowship: Cardinal Glennon
-
Kathy Monroe (1995) – Fellowship: UAB
-
Michele Nichols - Fellowship: Cincinnati Children’s
-
Rud Polhill
The division took over management of the Vestavia After Hours clinic in 1999, which later moved to Children’s South after its completion. Another major event for the division and the department occurred in 1999 when a contract was negotiated with Children’s Hospital and the HSF to assume the costs of the division, including all costs associated with the fellowship. The only costs not included were academic efforts that had no relation to Children’s and the provision of patient care services. The hospital billed for and kept the clinical revenue generated by the division and reimbursed the department for the difference between revenue and costs. This funds flow arrangement continues to date and has morphed to include the hospital covering most academic, outreach, clinical and administrative activities of the faculty.
-
-
2000s
Dr. Don Arnold, who had practiced pediatrics and consulted in child abuse cases in Florida for years, started his pediatric emergency medicine fellowship at UAB in 1999. Dr. David Bernard was his faculty mentor and they recognized the need for the standardized care of children brought to the ED with a complaint of concern for sexual abuse/assault. Given the large number of providers assessing these children, all with varying levels of experience and expertise, and the time it takes to appropriately evaluate these patients in a busy ED, an effective standardized care pathway required a circle the wagons approach. For his fellow quality improvement project, Dr. Arnold implemented a SANE (Sexual Assault Nurse Examiner) program in the ED, which reduced the number of providers seeing these patients to those specially trained to do so. Dr. Bernard took over when Dr. Arnold completed his fellowship and left for a faculty position at Vanderbilt University. In addition to training the nurse examiners, all examinations are videotaped and Dr. Bernard reviews each one to confirm the findings. Most recently, Dr. Bernard has expanded the training and oversight/peer review to other locations in the state. In 2004, he was also named the medical director of the CHIPS Center (Children’s Hospital Intervention & Prevention Services) where he sees patients referred to the outpatient clinic. He obtained AAP Sub-Board Certification in Child Abuse in 2013. Dr. Melissa Peters joined the faculty in 2004 after her pediatric emergency medicine fellowship at the Children’s Hospital of the King’s Daughters in Norfolk, Virginia. She was also passionate about providing expert care for children who are suspected of being physically abused and splits her time between the ED and CHIPS, becoming the medical director for Physical Abuse Services in 2004. She provides inpatient consultation for suspected child abuse and became board certified in Child Abuse in 2013. Dr. Cohen created a new Division of Child Abuse in 2015 and recruited Dr. Mike Taylor from the Medical University of South Carolina to become the new director.
In 2003 a major renovation of ED was completed increasing its size by 30%. Over 53,000 patients were seen in the ED that year. The fellowship was expanded to three positions per year in 2003.
The ED volume took an unexpected dip in 2004 to 46,000 patients seen. This was fortunate in some ways because resident coverage of the ED decreased by 2/3rds that year, marking the end of anything that resembled a resident run ED. To partially compensate for the decrease in ED providers, we began using nurse practitioners (NPs) that year. Though controversial at the time, the NPs have proven themselves as capable and valuable independent care providers. We started with three NPs and now have 15 with 24/7 coverage.The division expanded its clinical coverage in 2006 to include a deep sedation service for radiology patients. Dr. Jud Barber is the division’s director of Sedation and also chairs the hospital’s sedation committee. We continue to provide this service at Children’s South five days a week. 2006 also saw the creation of the Pediatric Simulation Center established at Children’s Hospital. Dr. Marjorie Lee White joined the faculty in 2008 after completing a combined critical care and pediatric emergency medicine fellowship and co-directed the Simulation Center with Dr. Nancy Tofil. Subsequently Dr. White became the assistant dean and vice president for Clinical Simulation for the School of Medicine and the UAB Health System and also holds the title of director of the UAB Office of Inter-professional Simulation for Innovative Clinical Practice, Center for Inter-professional Education and Simulation.
Dr. Stagno appointed Dr. Pete Glaeser as the vice-chair for Clinical Services for the department in 2008. He continues as division director and appointed Dr. Monroe as the medical director of the ED. Dr. Monroe had been the division’s research director, which was transitioned to Dr. Chris Pruitt, who joined the faculty in 2010 after completing his pediatric emergency medicine fellowship at UAB. Drs Monroe and Nichols continue as the pied pipers of resident and medical student research and outreach advocacy.
-
2010s
The division was honored in 2010 with the creation of the C. Phillip McWane Endowed Chair in Pediatric Emergency Medicine. Dr. Glaeser was named the first recipient of the chair.
The beautiful Benjamin Russell Hospital for Children opened in August of 2012. The new ED contains 53 rooms, including four major resuscitation areas in close proximity to a separate ambulance entrance, an elevator that goes directly to the heliport and radiology. This increase in capacity was predictably met with substantially increased ED volumes. The highest volume in prior years was 57,000 and we are now seeing 74,000 patients per year. Obviously this has required additional providers and faculty. The decision was made in 2017 to close the After Hours Clinic and use the pediatricians to staff the lower acuity area of the ED. Four specially designed rooms with their own nursing station and lockable entrances were created to care for the burgeoning number of patients presenting with behavioral and psychiatric complaints. Unfortunately, these complaints continue to expand far exceeding the four bed capacity and the lack of inpatient beds results in these patients being held in the ED, often times for days.
Current PEM Faculty
(year joined faculty)
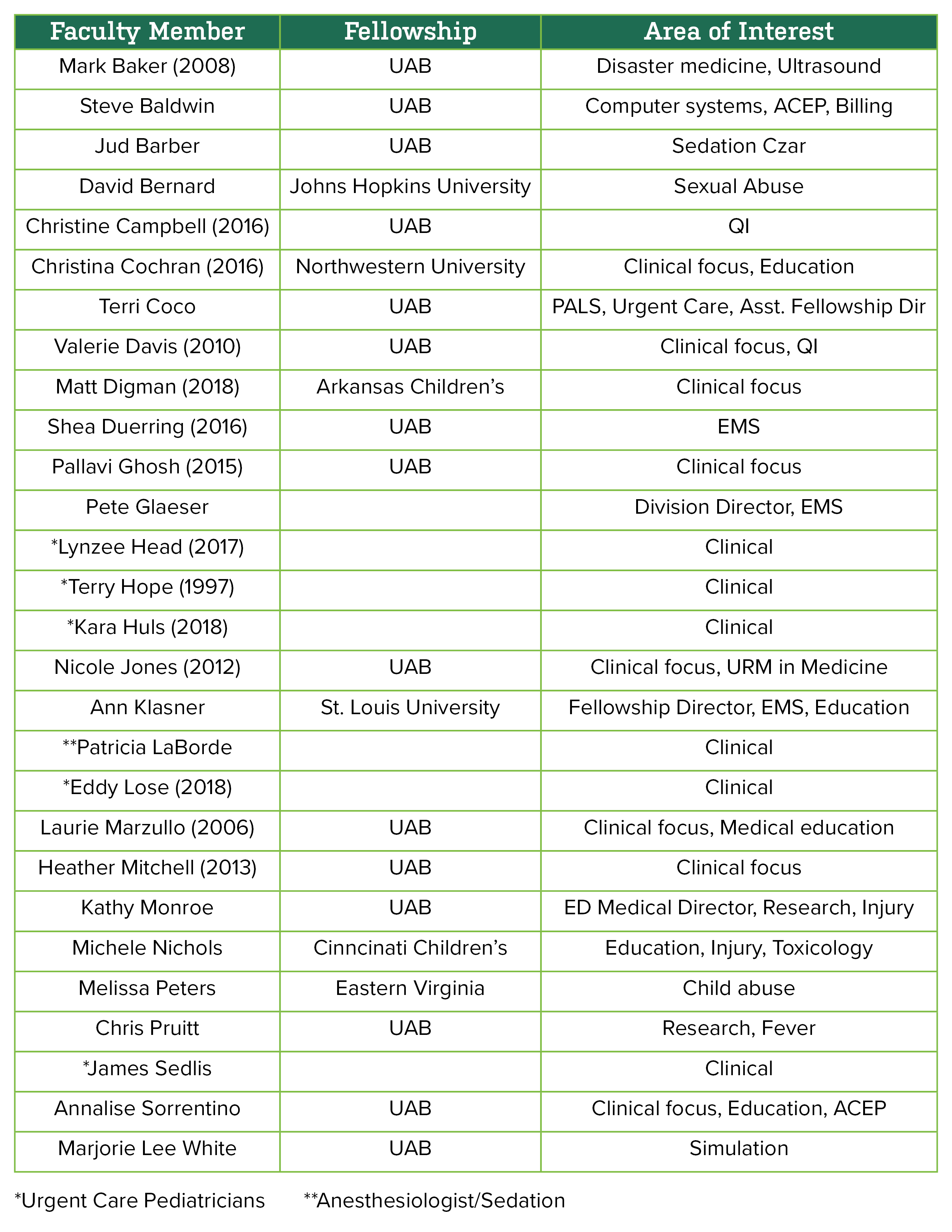
Additional division team members include: Jackie Freeman, Administrative Supervisor, Megan Beal, Office Associate II, Keandra Simmons, Office SVCS Specialist, Brittany Appelboom, Fellowship Program Coordinator, and Nipam Shah, Research Associate.
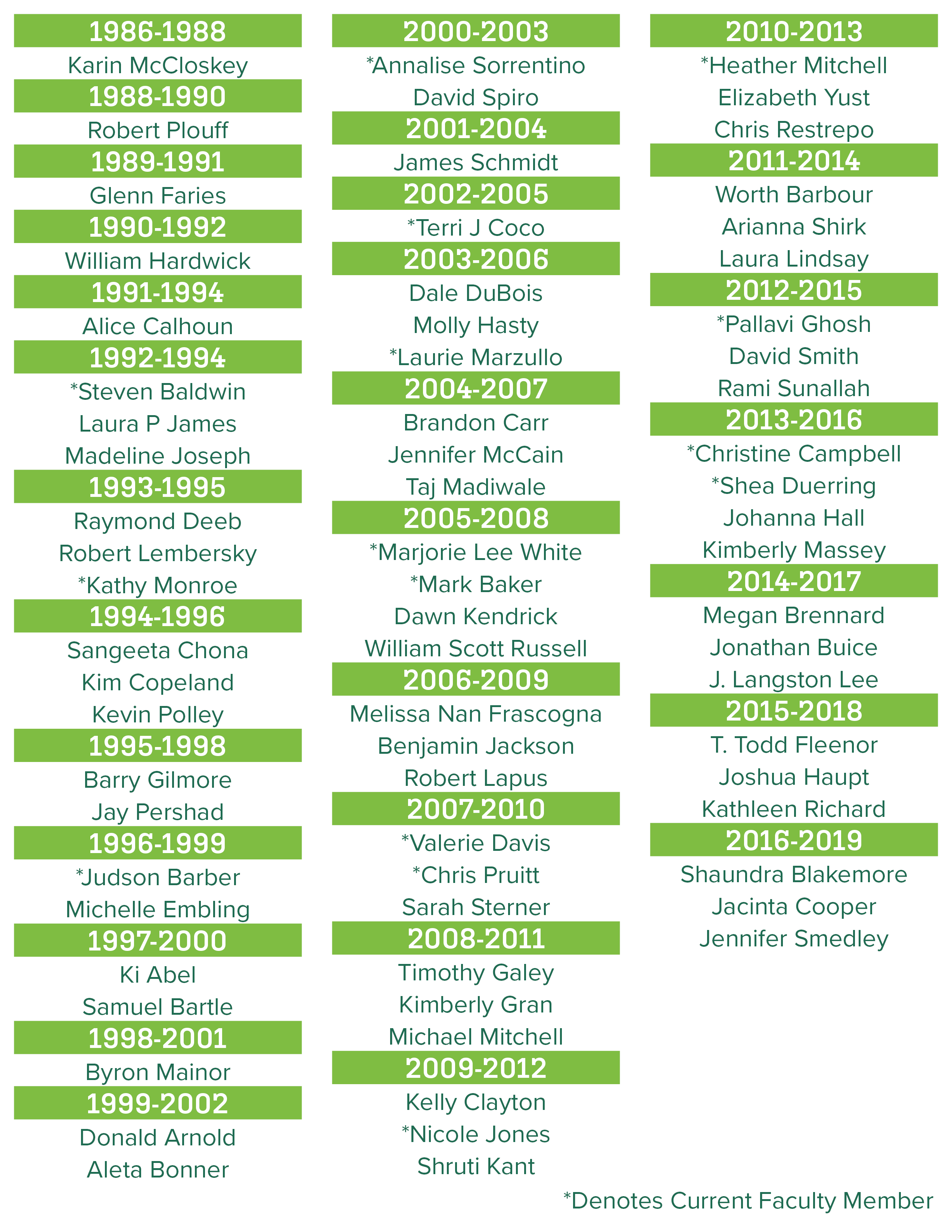
Fellows Who Have Trained With Us
Click here for a list with their current position