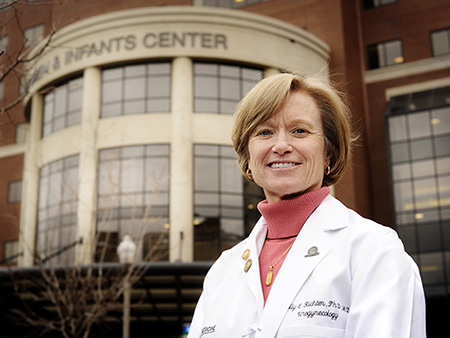
 Holly E. Richter, Ph.D., M.D.Holly E. Richter, Ph.D., M.D., director of Research in the University of Alabama at Birmingham’s Division of Urogynecology and Pelvic Reconstructive Surgery, has co-written two papers published in the Journal of the American Medical Association relating to urogynecologic surgery.
Holly E. Richter, Ph.D., M.D.Holly E. Richter, Ph.D., M.D., director of Research in the University of Alabama at Birmingham’s Division of Urogynecology and Pelvic Reconstructive Surgery, has co-written two papers published in the Journal of the American Medical Association relating to urogynecologic surgery.
SUPeR: Study of Uterine Prolapse Procedures
The SUPeR study was designed to determine whether treatment failure rates differed for vaginal mesh hysteropexy, a uterine conserving procedure, compared to a vaginal hysterectomy with suture apical repair, a typical surgery for uterovaginal prolapse. The randomized trial enrolled 183 postmenopausal women at nine clinical trial sites in the United States.
Uterine prolapse happens when a woman’s pelvic floor muscles and ligaments become weakened and stretch, ultimately causing a lack of support for the uterus; this can cause the uterus to slip out of the vagina.
Richter and co-authors determined that, of the participating women with symptomatic uterovaginal prolapse undergoing vaginal surgery, composite prolapse outcomes of those undergoing vaginal mesh hysteropexy did not differ compared to those of women undergoing a vaginal hysterectomy with uterosacral ligament suspension after three years. Further research will be needed to determine whether a vaginal mesh hysteropexy is more effective five and 10 years post-surgery.
ESTEEM: Effects of Surgical Treatment Enhanced with Exercise for Mixed urinary incontinence
The ESTEEM randomized clinical trial evaluated whether combining behavioral and pelvic floor muscle therapy with midurethral sling surgery was better than only a sling in treating women with moderate or severe stress and urgency urinary incontinence symptoms. Urinary incontinence, or loss of bladder control, affects up to 58 percent of women. Traditional midurethral sling surgery helps provide a backstop of support to a woman’s urethra for stress urinary incontinence, while pelvic floor muscle therapy exercises can be used to treat both stress and urgency urinary incontinence.
A total of 464 women were enrolled in the trial. ESTEEM’s findings showed that, for women with mixed urinary incontinence, behavioral and pelvic floor muscle therapy combined with midurethral sling surgery versus just surgery alone resulted in a small statistically significant difference in urinary incontinence symptoms at 12 months; but this difference did not meet the threshold for a clinically important difference.
“Both studies are prime examples of how continuous research through randomized clinical trials can help providers determine the most effective courses of treatment and therapy for women with urogynecology or pelvic reconstructive needs,” Richter said. “Being able to offer a full spectrum of treatment options to women is imperative, and our ongoing research at UAB helps us better care for each woman’s individual needs.”