Media Contact: Adam Pope
 Early results from the United Kingdom's RECOVERY trial this summer were a welcome piece of good news in the midst of the COVID-19 pandemic. Critically ill patients on ventilators who received dexamethasone, a corticosteroid drug, were at a one-third lower risk of dying than those who did not receive the drug. Patients receiving oxygen therapy, but not on ventilators, had a 20% lower risk of dying. Nature, the scientific journal, called it a "coronavirus breakthrough."
Early results from the United Kingdom's RECOVERY trial this summer were a welcome piece of good news in the midst of the COVID-19 pandemic. Critically ill patients on ventilators who received dexamethasone, a corticosteroid drug, were at a one-third lower risk of dying than those who did not receive the drug. Patients receiving oxygen therapy, but not on ventilators, had a 20% lower risk of dying. Nature, the scientific journal, called it a "coronavirus breakthrough."
Better yet, as Nature noted, dexamethasone is both cheap and commonly used. The trouble is, "dexamethasone is already in short supply," said Randy Cron, M.D., Ph.D., professor of pediatrics and medicine at UAB. So Cron and Winn Chatham, M.D., professor of medicine at UAB, are conducting a pilot study of another corticosteroid, methylprednisolone. Outside of COVID-19, oncologists often use dexamethasone to treat hemophagocytic lymphohistiocytosis, a cytokine storm syndrome seen in patients with blood cancers such as leukemias and lymphomas. Rheumatologists such as Cron treat cytokine storm syndrome (where it is commonly called macrophage activation syndrome) in patients with lupus and rheumatoid arthritis using methylprednisolone.
"Methylprednisolone is more readily available than dexamethasone," Cron said. "The thought is if both are equally effective, then physicians can use what is available to them to treat COVID-19 cytokine storm syndrome." And, "by implication, other glucocorticoids will likely be equally effective at the glucocorticoid equivalent dosing."
|
UAB urgent research grants against COVID-19 This study is one of 10 pilot projects recently funded by $402,000 in donations as part of the second round of UAB's urgent, high-impact COVID-19 grant initiative. This follows 14 projects funded in the first round of urgent, high-impact COVID-19 grants. |
COVID-19 and cytokine storm
Cron is a leading expert on cytokine storm syndrome, a potentially life-threatening overreaction by inflammatory immune proteins known as cytokines. (In 2019, he published the first textbook on cytokine storm syndrome.) "Cytokines are there to fight off infections and ward off cancers," Cron said. "But when they are out of control, they can make you very ill."
Anyone battling a serious infection, regardless of cause, may experience a cytokine storm, Cron said. In addition to blood cancers and rheumatic diseases, cytokine storm syndrome is seen in herpes virus family member infections, and case reports have noted nearly 100 different infectious agents that can cause cytokine storms. In patients with COVID-19, clinicians increasingly see cytokine storm syndrome as a major factor in poor outcomes. Cytokine storm syndrome develops in a large percentage of COVID-19 patients who are ill enough to require hospitalization, Cron said.
Why glucocorticoids?
Glucocorticoids, such as dexamethasone and methylprednisolone, are both "used to calm the cytokine storm," Cron said. "They have very broad-ranging effects on the immune system," including decreasing production of pro-inflammatory proteins and "decreasing function of multiple immune cell types."
In a pilot project that was one of 10 recently funded by UAB's urgent, high-impact COVID-19 grant initiative, Cron and Chatham, plan to enroll at least 30 patients hospitalized with COVID-19 pneumonia who have features of cytokine storm syndrome.
The World Health Organization initially recommended against use of glucocorticoids in treating COVID-19 because studies of their effectiveness when used against coronaviruses in SARS and MERS outbreaks had varying results, and glucocorticoids increase the risk of secondary infection in patients. "Nevertheless, out of desperation, many overwhelmed centers have resorted to glucocorticoids in treating COVID-19 cytokine storm syndrome," Cron and Chatham wrote in their project proposal, and early reports "have shown promising results." These drugs' effectiveness at calming cytokine storms means the benefits of short-term use outweigh concerns about secondary infections, Cron said. "They can be tapered over time to keep the cytokine storm syndrome under control while the patient improves clinically and by lab markers of disease," he said.
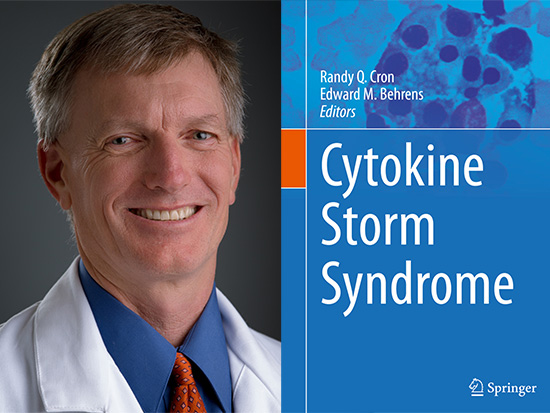 Randy Cron, M.D., Ph.D. (above) wrote the first textbook on cytokine storm syndrome in 2019. Cron and UAB's Winn Chatham, M.D., are testing another potential treatment for cytokine storm syndrome in COVID-19: a targeted drug called anakinra.Study details
Randy Cron, M.D., Ph.D. (above) wrote the first textbook on cytokine storm syndrome in 2019. Cron and UAB's Winn Chatham, M.D., are testing another potential treatment for cytokine storm syndrome in COVID-19: a targeted drug called anakinra.Study details
Patients in the study will be randomized to receive either 6mg daily of dexamethasone or 32mg daily of methylprednisolone. The goal is to reduce the need for invasive mechanical ventilation and ICU care. "We believe methylprednisolone will minimize ICU admissions and enhance survival," wrote Cron and Chatham in their project proposal.
Methylprednisolone and dexamethasone have similar side-effect profiles, "but are often used at different glucocorticoid equivalent dosing" — methylprednisolone tends to be used at higher doses — "and they have different pharmacokinetics, which has implications for tapering dosing when patients are recovering," Cron said.
Patients will receive the drugs at the doses listed above for seven days or until they show stable improvement in oxygen saturation and lower levels of markers of cytokine storm syndrome, including serum ferritin, D-dimer and C-reactive protein.
Genetic signatures for cytokine storm syndrome in COVID-19?
|
"Methylprednisolone is more readily available than dexamethasone. The thought is if both are equally effective, then physicians can use what is available to them to treat COVID-19 cytokine storm syndrome. And, by implication, other glucocorticoids will likely be equally effective at the glucocorticoid equivalent dosing." |
The researchers also plan to explore genetic risk factors that may be shared by COVID-19 patients who develop cytokine storm syndrome. Cron and colleagues have identified genetic risk factors in other cytokine storm syndromes, including those triggered by H1N1 influenza. This earlier work suggests that as much as 15% of the general population carries genetic mutations putting them at higher risk for developing cytokine storm syndrome. Finding such risk factors in COVID-19 patients would allow clinicians to target treatments to patients with the highest potential for success on those therapies.
Cron and Chatham are co-principal investigators on the methylprednisolone study, which also includes Devin Absher, Ph.D., of the HudsonAlpha Institute of Biotechnology, where whole genome-sequencing of patients will be done.