 Screening for cancer-causing infections such as human papillomavirus (HPV) can be challenging in developing countries when access to health services is limited. But in Nepal, where high-risk HPV is prevalent, UAB research demonstrates that self-collected samples can be effective for screening.
Screening for cancer-causing infections such as human papillomavirus (HPV) can be challenging in developing countries when access to health services is limited. But in Nepal, where high-risk HPV is prevalent, UAB research demonstrates that self-collected samples can be effective for screening.
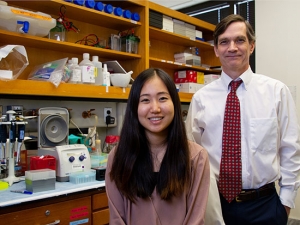
Sadeep Shrestha, Ph.D., associate professor in the Department of Epidemiology, is the senior author of the new study published to PLOS ONE that investigated HPV prevalence and screening methods in Accham, a remote district in Nepal’s Far-Western Region.
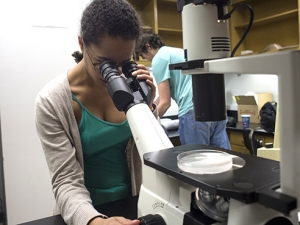
During a one-day health camp at the Nepal Fertility Care Center, the team gathered clinician- and self-collected cervical specimens among women with little or no formal education to test whether or not the latter were comparable to clinician’s specimens for the purposes of screening.
“We learned that, even in a remote area among illiterate women, self-collected samples for HPV and cervical cancer screening is feasible,” Shrestha said. “Most of these participants had never visited a medical center, and thus an efficient sampling scheme will be needed for HPV/cervical cancer screening purposes.”
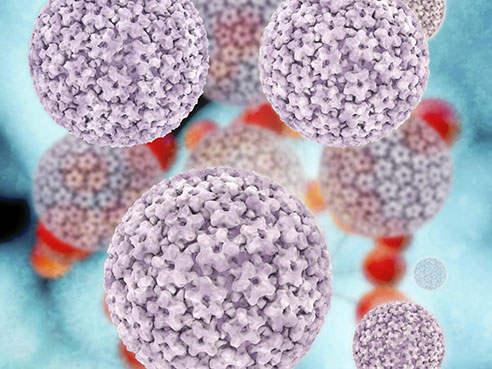
Nearly all cases of cervical cancer are believed to be caused by HPV infection, and around 85 percent of the more than 270,000 deaths annually attributed to cervical cancer are in developing countries, according to the World Health Organization. The incidence of cervical cancer in Nepal is 24.2 per 100,000, one of the highest rates in South Asia.
Shrestha says the prevalence of high-risk, cancer-causing HPV was 9.6 percent among the women who attended the one-day camp and at least 25 percent had abnormal cytology. But that estimate may be low.
| Nearly all cases of cervical cancer are believed to be caused by HPV infection, and around 85 percent of the more than 270,000 deaths annually attributed to cervical cancer are in developing countries, according to the World Health Organization. The incidence of cervical cancer in Nepal is 24.2 per 100,000, one of the highest rates in South Asia. |
“We realized that many other women could not attend the health camp due to distance to the camp, potential health issues or even because of cultural taboo,” Shrestha said. “Because of these factors, we believe that the prevalence of HPV in our study is an underestimate. This region has a high prevalence of HIV, and therefore we believe this region could also have a high prevalence of HPV; but multiple camps and creative designs to enroll women will be needed to prove this.”
Shrestha says that a limited budget meant a limited sample size; however, this was the first HPV and cytology study conducted in rural Nepal, so its results should be considered useful.
“The model of putting screening projects into existing health camps, coupled with a self-sampling approach to HPV, would be beneficial for the Nepalese government with its comprehensive screening plans,” Shrestha said.
The infrastructure for testing for HPV in Nepal is not fully developed, so these samples were tested in the United States, Shrestha says. The development of better local testing facilities in Nepal would help improve the sustainability of routine HPV testing in the future.
Derek Johnson, a doctoral student in the Department of Epidemiology and first author, stayed in Nepal for 18 months to help conduct the study.