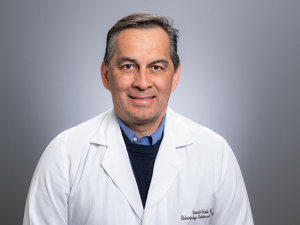
By giving every part of a team a voice, 3D Problem-Solving consistently replaces frustration with fulfillment. Especially since the pandemic began, “people are frustrated and burned out,” said Rick van Pelt, M.D., Chief Clinical Transformation Officer for UAB Medicine and UAB Hospital. “We leverage that emotional energy and use it to identify where we need to work and provide support.” STEVE WOOD | University RelationsWhat would you change about your workplace? If you didn’t have to consider org charts or business as usual, that is — if your only parameters were to find the best way possible to do the work, and maximize job satisfaction for everyone on your team?
By giving every part of a team a voice, 3D Problem-Solving consistently replaces frustration with fulfillment. Especially since the pandemic began, “people are frustrated and burned out,” said Rick van Pelt, M.D., Chief Clinical Transformation Officer for UAB Medicine and UAB Hospital. “We leverage that emotional energy and use it to identify where we need to work and provide support.” STEVE WOOD | University RelationsWhat would you change about your workplace? If you didn’t have to consider org charts or business as usual, that is — if your only parameters were to find the best way possible to do the work, and maximize job satisfaction for everyone on your team?
That is the offer Rick van Pelt, M.D., and his team in Clinical Practice Transformation (CPT) make to units across UAB Hospital. CPT serves as a kind of internal consulting group, part of the operations arm of the hospital, with a goal of “rethinking how care is delivered on the front lines,” said van Pelt, whose title is chief clinical transformation officer for UAB Medicine and UAB Hospital.
In a short two years, the CPT team has sparked sustainable change in more than a dozen clinical units that is easily visualized on graphs of average patient length of stay and other key hospital metrics. In Hepatology, for example, patient depart efficiency improved by 295 percent from their primary unit, GI Surgical Oncology, after CPT arrived. In Renal Transplant, the average length of stay for fresh kidney transplants decreased by 1.38 days. But charts and data are not the only reason there is a waiting list to engage CPT. The team’s unique approach, which they call 3D Problem-Solving, taps into the emotions of the care team before anything else. It has attracted glowing testimonials that include phrases such as “not seen anything like this,” “wonderful process” and “I have been amazed.”
It has also attracted new staff — one of the clinicians on the CPT team was so impressed with what happened on his unit that he now divides his time between patient care and internal consulting. “There is nothing else like it that we are aware of,” said that physician, David McCollum, M.D., a hospitalist who is an assistant professor in the Department of Medicine. By giving every part of a team a voice, 3D Problem-Solving consistently replaces frustration with fulfillment. “Once people understand this is possible, they are on board,” McCollum said. “It’s really a wellness thing for doctors, nurses, everybody.”
“When I learned that CPT would be working with our interdisciplinary neonatal team, I wasn’t sure what to expect. I can’t say enough good things about this team. They are caring, professional and skilled and bring a new and refreshing approach to problem-solving and project management. I have been amazed at how much we have accomplished in a short amount of time. The CPT team values all stakeholders and is focused on improving operations. I am grateful to have them working with us and look forward to all that will be accomplished in the future.”– Donna Purvis, R.N., nurse manager, UAB Regional Neonatal Intensive Care Unit
‘Where is your pain?’
“We are often invited into areas with longstanding challenges,” van Pelt said. He is an anesthesiologist by training who became heavily involved in care redesign while in practice, got an MBA at Harvard and later became a consultant focused on improving the delivery of health care. After an engagement at UAB, he was hired to lead CPT in 2019. “We are usually not the first group that has come in, either,” van Pelt said.
But CPT is almost certainly the first group that has actively sought out the warts and walls and wounds that lurk inside even high-performing teams, and the first group that has made it clear they are not bringing the solution with them. “People say, ‘We have no control over it, so we can’t fix it,’” van Pelt said. “We say, ‘Let’s go there. Let’s uncover the mess and arrive at the answer through understanding.’ We start with the view that the people who understand the problems are the ones doing the work, the front-line folks.”
Especially since the pandemic began, “people are frustrated and burned out,” van Pelt said. “We leverage that emotional energy and use it to identify where we need to work and provide support.” His team has the institutional position and experience to help groups make the business case for major change, if needed — including getting the OK to hire personnel, redefine longstanding processes and shift pain points that staff have always considered to be off limits.
“When you go to the doctor, the first question they ask is, ‘Where is your pain?’” van Pelt said. “We are here to take care of your pain. We let them know, ‘We care about you and your well-being.’ This is about emotional support as well as addressing the system.” Familiar process-improvement models such as Six Sigma are built on the intellectual foundations of systems theory and participatory management theory, van Pelt says, and 3D Problem-Solving incorporates these as well. “Our differentiator is that we add peer support theory — there is a team element to everything we do,” van Pelt said.
Although 3D Problem-Solving was developed for health care, “we think it will work in any setting,” van Pelt said. His team is working with UAB’s Harbert Institute now to license 3D Problem-Solving widely. “These principles can scale,” he said.
“People say, ‘We have no control over it, so we can’t fix it.' We say, ‘Let’s go there. Let’s uncover the mess and arrive at the answer through understanding.’ We start with the view that the people who understand the problems are the ones doing the work, the front-line folks.”– Rick van Pelt, M.D., Chief Clinical Transformation Officer for UAB Medicine and UAB Hospital
Redesigning trauma
An example is in order. One of CPT’s first clients was UAB’s trauma service, ground zero for the victims of the most gruesome car wrecks, gunshot wounds and other catastrophic injuries in Alabama and beyond.
When UAB fills up, trauma patients must be diverted to hospitals farther away or to facilities that cannot offer the same standard of care. “We are the leaders in trauma in Alabama,” McCollum said. “If we are in overload, that is a huge problem for the state.” Shaving fractions of a day off the average length of stay for trauma patients can have major effects across Alabama, he notes.
Working with the front-line teams in trauma, CPT helped identify a completely different way to move patients through the service. The change required hiring 12 additional advanced practice providers (nurse practitioners or physician assistants) — but it decreased the average length of stay by 1.4 days. The trauma service was able to admit 46 more patients per month and hit 583 percent of the break-even figure needed to justify hiring those 12 advanced practice providers.
“The Clinical Practice Transformation process was vital to our trauma service redesign,” said Jeffrey D. Kerby, M.D., Ph.D., Brigham Family Endowed Professor and director of the Division of Trauma and Acute Care Surgery. “We had previously attempted this on our own and had never been able to achieve long-term success. Through engagement of all stakeholders on the service and identification of key measures of success, we were able to work through the steps necessary and obtain needed resources to achieve a successful reorganization of the service. We have been able to exceed expected decreases in patient length of stay while improving our quality of care. This has allowed us to decrease diversion rates and keep our trauma center open continuously as a valuable resource to our community.”
But where did the idea come from? Why did CPT succeed when previous efforts had not? The solution emerged through CPT’s 3D Problem-Solving process, van Pelt explains. “The biggest change is it was a unit-based service that became a platform-based service,” he said. “They introduced three teams to cover the units in trauma simultaneously. That involved not only restructuring but adopting a new mental model. You have to get past ‘we have never done this before.’”
“We had previously attempted this on our own and had never been able to achieve long-term success. Through engagement of all stakeholders on the service and identification of key measures of success, we were able to work through the steps necessary and obtain needed resources to achieve a successful reorganization of the service.... This has allowed us to decrease diversion rates and keep our trauma center open continuously as a valuable resource to our community.”– Jeffrey D. Kerby, M.D., Ph.D., Brigham Family Endowed Professor and director of the Division of Trauma and Acute Care Surgery
Discover – Distill – Define
The 3D approach begins by gathering leaders of every discipline in the unit — physicians, nurses, pharmacists, therapists, care transitions — along with two members of the CPT team: a facilitator and a scribe.
“The first step is to recognize that the traditional silos between clinical and operational environments need to be broken down,” van Pelt said. “Everything is connected — and the silos are how you end up with subsequent dysfunction. Problems that start on the front line go everywhere: pharmacy, transport, supply chain. We are multidisciplinary and very system-based. We are not about course-correcting individual behavior but addressing the entire system.”
These sessions “usually include about 15 people,” said Anyet Belyeu, DNP, CPT’s clinical director. “The entire process is about team-building, as well as gathering input.” The facilitator begins with a question: What are the issues and concerns with delivering exceptional care on this service?
This initial brainstorming session is the first of the three D’s: discover. “This is how we determine the current state, and determine where we need to look, so we can focus on things that need attention to reach the future state,” van Pelt said. “A lot of times, the future state is imposed from above on situations that are not well understood. We are trusting the collective genius of the group. There is an incredible synergy that happens.”
Everyone is engaged in the conversation, with the CPT scribe capturing every statement. “It is team-building, not just extracting information,” van Pelt emphasized. “Frustration comes out. You get a big mix of things. People are being heard, maybe for the first time, and we are capturing everything everyone is saying.” The facilitator makes sure that there is no finger-pointing or jumping to solutions. “We take that phase to exhaustion, until everything has come out,” van Pelt said. “We boil them down to tweet-sized statements, not monologues.”
The CPT team usually ends up with anywhere from 70 to 150 of these statements, then coalesces these elements into groups. This is the second D: distill.
Then it is time for the final D: define. “We usually get five to eight themes that have emerged,” van Pelt said. “We ask, ‘If we could do only one, which would we focus on?’ Having to identify what matters most gets you to the critical 20 percent.” That is the Pareto Principle, also known as the 80-20 rule, which says that 80 percent of outcomes are due to 20 percent of causes. “That becomes the starting point, so we are always working on what matters,” van Pelt said. And, critically, these are the problems that matter to everyone. The one to three themes that make it to the critical 20 percent must be chosen by unanimous vote from the group.
“I have been here 16 years, and I have not seen anything like this,” said Rachel A. Martin, MSN, R.N., a nurse manager in the Comprehensive Transplant Institute, another CPT client. “It is so great to bring disciplines together and fix things fast.”
“Accountable care teams join leaders with the front line who are vested in taking care of patients, gives us a common platform to come up with solutions and enhances our ability to deliver team-based care to our patients. It has really helped our patients by providing better quality of care, greater engagement with their care team and overall improved outcomes.” – Shikha Mehta, M.D., associate professor of medicine and associate medical director for Kidney Transplant
‘Everyone’s voice is equal’
CPT specializes in developing accountable care teams. Often referred to as ACTs, these are a research-backed model for providing inpatient care in which teams are led by a triad of a physician, nurse manager and operations personnel, who receive leadership training. They also include a broader team that is trained in systems thinking and problem-solving and has access to unit-level metrics to guide performance improvement. The group meets weekly to focus on performance-improvement projects. “They pick an initiative, we guide them through that, then they are ready to move on to the next initiatives on their own,” van Pelt said. As of November 2021, CPT has worked with 10 units to transition them to an ACT model, with another seven on deck.
“It is great to have an arena where everyone’s voice is equal,” said Jaclynn Gothard, R.N., a leader in the Care Transitions discipline, which helps patients as they are being discharged from the hospital. “It has brought us into a progressive place and a place of shared governance. ACTs are a wonderful process that grows leadership.”
Research led by UAB’s Katherine Meese, Ph.D., assistant professor in the Department of Health Services Administration in the School of Health Professions, has quantified the beneficial effects of ACTs. In a paper presented at the European Academy of Management conference in June 2021, Meese and co-authors studied scores from a Health System-wide survey of employee well-being during COVID. Members of ACT units “felt more supported by the organization, had a better sense of community at work, and were less likely to report loneliness and social isolation as a major stressor,” the authors noted.
In addition to accountable care teams, CPT conducts clinical/operational redesigns, as in the trauma service example above, which are “larger scale,” van Pelt said. His team also takes on signature projects, which tend to come up “when hospital operations needs help with a fire that can’t be put out in the typical way,” van Pelt said. That has certainly been the case during the COVID pandemic, in which the CPT team has led projects on clinical standardization, glove conservation, discharge education and lab/supply chain synergy, among others.
In each of these engagements, 3D Problem-Solving plays a central role. “There is nothing else like it that we are aware of,” McCollum said. “By the time we get to implementation, the front line is feeling really good. They see dramatic improvement, and they can’t imagine practicing without it.”