 |
Gorgas Case 2003-08 |
 |
|
The patient was seen by the Gorgas Course participants in the outpatient department of the Tropical Medicine Institute.

 History: 46-year-old female with a 5-day history of an extensive and progressive painful right arm lesion with small papules. She initially had a sudden onset of sharp pricking stinging pain near the elbow with a fever of 38°C and sweats the first night after onset. By the next day she noticed an erythematous lesion that progressed down to the wrist over the next 4 days despite the ingestion of acetominophen, dexamethasone, and antihistamines. The fever disappeared after the first day but the pain and edema in the arm increased. No similar episodes in the past and no significant past medical history. No history of recent trauma to the area. On no regular medications. Epidemiology: Urban dweller from Lima and grew up in an urban setting in the coastal city of Chiclayo. Single and unemployed. No TB or HIV contacts or risk factors. Physical Examination: Afebrile, normotensive in no distress. Abnormalities restricted to a marked erythematous reaction over the right arm extending to the wrist with small red papules near the elbow [see Image A]. Laboratory Examination: Hematocrit normal. Urinalysis normal
|
|
Diagnosis: Necrotic arachnidism due to bite of the South American recluse spider Loxosceles laeta.
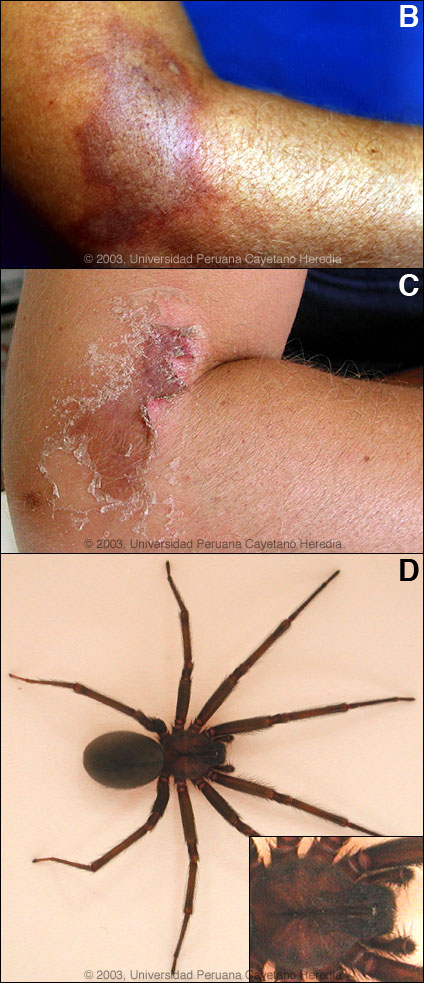
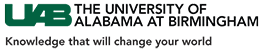
 Discussion: The patient was begun on analgesics, clindamycin, and ciprofloxacin, and over the next week the lesion evolved to the classical violaceous plaque with a pale center and blisters [see Image B] surrounded by a typical erythematous halo. A white ring of vasospasm and ischemia may be seen between the central violaceous lesion and the halo, but was not present in this case. The violaceous central plaque represents an area of hemorrhage and thrombosis which in more severe cases will progress to frank necrosis. In retrospect, the patient could associate the exact time of sudden onset of pain with a probable bite event but as is common, she never saw the spider. The patient was seen again 2 weeks after initial presentation with good resolution of the wound [see Image C]. The diagnosis of loxoscelism is a clinical one. The spectrum ranges from a mild skin irritation, to severe local necrotic reactions, to a less common syndrome (10-15% of cases) of viscerocutaneous loxoscelism manifested with dramatic hemolysis and renal failure. Mortality in severe cases is higher in children due to lower body weight per amount of venom injected. The erythematous margin of the cutaneous lesion spreads irregularly, influenced by gravitational factors as venom spreads in a manner related to the body part affected. The most severely affected part of the lesion may be eccentrically placed towards the area of the original bite. In severe cases a hemorhagic bulla will form within a few days which will then evolve to the frank eschar. In contrast to anthrax, the borders are irregular, ill-defined and without the significant edema right around the edges of the lesion usually seen in anthrax. Anthrax lesions are painless; loxoscelism is always painful. The bite of Loxosceles laeta is thought to cause more edema but is less often necrotic when compared to the related and well-studied brown recluse spider Loxosceles reclusa found in the United States. In Perú, as in many other countries that have various Loxosceles sp., Dapsone is administered at 100 mg/day for 1 week unless patients already have active hemolysis or are G6PD deficient. No large controlled trials have been reported, but clinical experience and several limited studies support this practice. Dapsone was not available at the time this patient presented, otherwise it would have been prescribed. Systemic corticosteroids are only advised in cases with facial lesions. Patients with any evidence of hemolysis or hemoglobinuria require vigorous intravenous hydration and urinary alkalinization. Aggressive debridement and escharectomy is usually advised once the acute phase is over. Work in animal models has shown anti-venom to be effective if administered in the first 12-24 hours after a bite. There is no commercial product available in North America. In Perú a polyvalent equine antiserum raised against Loxosceles laeta and Loxosceles rufipes is produced by the NIH-Perú. It is administered subcutaneously once, 10 ml for adults 5 ml for children. Loxosceles laeta accounts for 98% of loxosceles cases in Perú, but is only seen in coastal regions and up to 1,200 m in the Andes but never in the jungle regions. They live most commonly in very domestic environments in both urban and rural areas, often hiding in clothing in drawers or in closets. They are not agressive and only bite when disturbed or threatened. Bites occur more commonly in summer (January-April) when the spider reproduces and most bites occur at night or in the early morning. At least 54 species of Loxosceles are described from North and Central America and 30 from South America. Loxosceles laeta is native to Perú, Chile, Ecuador, Argentina, Uruguay, and south and eastern Brazil. It has been accidently introduced into the U.S. and several Central American countries at various times but does not naturally thrive in those locations. Loxosceles laeta is similar in appearance to other recluse spiders but is generally larger with a body length up to 15 mm [see Image D]. The head region has dark violin shaped markings on the dorsal aspect [see inset in Image D] but these markings cannot be reliably used to identify recluses as other types of spiders may have similar markings.
|