Integration of CME Services, Resident Education, and Quality Improvement Efforts
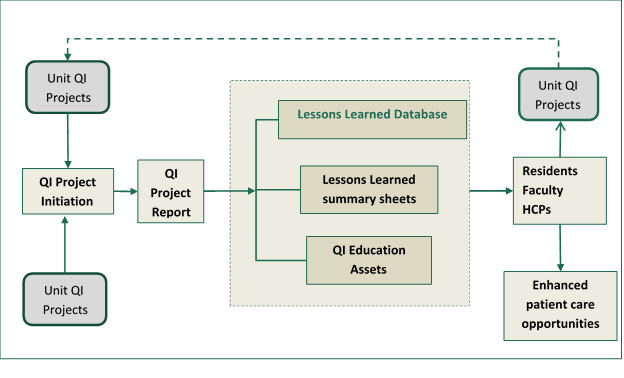
A quality improvement lessons learned database provides an opportunity to integrate existing quality improvement education, frameworks, and assets into resident education requirements and can provide a platform for developing both discrete and longitudinal QI initiatives that may serve as a component of service for faculty P&T portfolios and ultimately identify actions than positively impact patient health and quality of outcomes.
The system will also serve as a mechanism for disseminating a standard framework for approaching quality improvement initiatives and a searchable database for supporting identification of approaches, tools, and techniques to QI projects.
-
Summary
-
Current Situation
Current Situation
Resident quality improvement projects are completed for most residency programs. Currently, information generated by these projects tends to be siloed within departments, and knowledge gleaned from these projects has a limited distribution.
-
Goals
Goals
- Develop a Quality Improvement initiation tool to help residents formulate projects
- Develop a searchable lessons learned database to capture the results of concluded QI projects initiated by residents
- Integrate information on health care and hospital metrics that serve as starting points for project development
- Curate the database to develop the resources and skill sets needed to provide a range of support services to UAB resident programs, PI CME projects, and help build a mature system with continuous incremental improvement and knowledge management capability.
-
Process
Process
Use the lessons learned database to aggregate information that directly supports resident education objectives, health system objectives, codify the process, knowledge set, and structures used and incorporate them into a repeatable QI process that will provide value to internal customers.
-
Long-Term Objective
Long-Term Objective
- Add value to departmental and divisional quality improvement efforts by providing a range of support and organizational services that can facilitate and enhance quality improvement efforts
- Codify good practice to facilitate organizational knowledge management growth and effectiveness
- Develop and extend the internal capability of the UAB office of CME so that it can serve as a resource for individual doctors who must meet CME and MOC requirements
-
Current Situation
-
Anticipated Benefits
Benefits to resident program directors Benefits to UAB residents - Opportunity to develop and track longitudinal projects
- QI instructional support
- Opportunity to align resident interests with projects
- Documented attainment of AGME learning objectives
- Opportunity to create research agenda around QI projects
- Access to previous studies conducted by resident
- Enhanced access to QI tools and resources in context
- Potential to work within an existing QI framework
- Potential opportunity to develop publishable content
Benefits to UAB faculty Benefits to Health system/units - Support teaching and service components of promotion & tenure proposals
- Increased job and unit-specific knowledge
- Engagement in meaningful projects that advance personal and unit goals
- Alignment of certification requirements with work schedule
- Support data-driven approach to grand rounds content development
- Increased quality of outcomes
- Improved patient care
- Increased employee engagement
- Enhanced employee alignment
- Cost reduction
- Internal QI knowledge base
- Inform strategic planning efforts
- Increase publication output
-
Action Plan
- Identify specific assets that would be useful to residents in completion of a QI project through:
- Consultation with Quality Academy faculty
- Program director/QI facuty perspectives [Draft]
- Needs assessment of resident groups [Draft]
- Revise and deploy existing education assets as individual knowledge objects in an accessible environment
- Develop a Proejct initiation template based on stakeholder feedback
- Require residents to fill out the template as a starting point for each QI project
- Initiate pilot with department/division resident group
- Assess results, complete modifications, redeploy with additional pilot group
- Identify specific assets that would be useful to residents in completion of a QI project through:
-
Structure
-
Basic Elements
Basic Elements
A searchable database framed by analysis of resident needs containing:
- Modular quality improvement education assets
- Quality improvement tools, templates, and frameworks
- Lessons learned reports from previously conducted QI projects
- Integration with existing commonly accessed systems
-
Conceptual Design
Conceptual Design
-
Basic Elements
-
Expected Outcomes
A system that creates a shared mental model of the UAB institutional approach to quality improvement fostering:
- Localized learning
- Empowerment and alignment of QI teams
- Longitudinal project tracking
- A CME-curated system that provides unit feedback and identifies educational needs along with mechanisms to:
- Add value to departmental and divisional QI efforts
- Codify good practice to facilitate organizational knowledge management
- Serve as a resource for individual CME and MOC requirements
- Communicate processes, tools, and techniques to enhance patient outcomes
-
Template
Project Title Title of the project Project Team Identify project team members Issue Primary problem identified and addressed by the team Primary Objective Define the specific aim of the project in terms of how it will impact the employees, service, or process being examined – e.g. reduce cost; improve productivity; support strategy; facilitate operations; increase flexibility; integrate services; generate revenue Scope Define the work involved, expected output(s), and limits of the project Length Project duration (estimated hours of work) Metrics Define measurements of success Data Collection - Type
What type of data will be collected? Qualitative [nominal, ordinal, binary]; Quantitative [discrete, continuous]; input? Throughput? Output?
Unit of analysis- Method
How will the team collect the data needed? Chart review? Survey [paper or online]? Observation? Interview/focus group? - Access
Who controls the data and how will the team gain access? - Issues
What issues are associated with data access/collection that might need to be addressed? Results What are the intended project outcomes Identify potential QI tools Cause-and-effect diagram; process map; why-why diagram; histogram; scatter diagram; Control chart run chart [click for an example of linked education asset], variables chart, attribute chart]; force-field analysis; Pareto chart; Failure Modes and Effects Analysis Components to be included in Final Report Lessons learned: [Included as part of a Final report to the program director What went well?
What didn't go well or had unintended consequences?
If you had it all to do over again, what would you do differently?
Can the primary lessons learned be classified according to core competencies:o patient care o medical knowledge o team performance o patient outcomes o system-based practice Indicators of success for future similar projects Suggestions for avoiding issues that impacted the effectiveness of the project Resources used/helpful resources/resources needed for future similar projects What recommendations would you make to others doing similar projects?
Recommendations for next implementation·
Recommendation for policy, procedure, or training
Is there a policy or policy change recommendation you would make based on your findings?