 |
Gorgas Case 2005-02 |
 |
|
The following patient was seen in the outpatient department of the Tropical Medicine Institute.
 History: 66 yo female diabetic with 2 weeks of progressively worsening RUQ pain, fever, chills and some episodes of diarrhea. No previous surgical history.
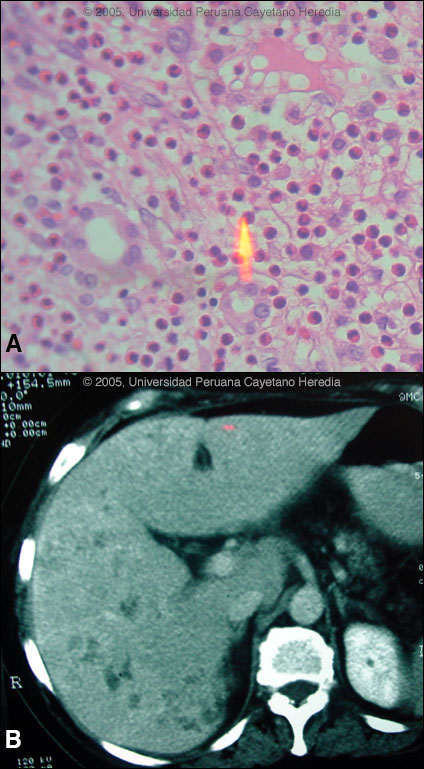
Epidemiology: From agricultural community in Ancash high in the Andes. Diet based mainly on vegetables and grains. No TB exposure. No significant ethanol intake. Physical Examination: (on transfer to Lima): Fever, RUQ rebound (positive Murphy's sign). Chest clear. No splenomegaly or lymphadenopathy. Stool heme negative. No rash. Laboratory Examination: Hb 11.5. WBC 16,500 with 25 neutrophils, 4 bands, 10 lymphs and 63 eosinophils. Both transaminases and alkaline phosphatase 3X normal. Bilirubin 1.8. Negative blood cultures. Negative serology for typhoid and brucella. Negative stool for O & P. Abdominal echo with 1 small stone in the gall bladder with no inflammatory changes. The patient was admitted to the surgical service and given intravenous antibiotics for 3 days without resolution of fever or symptoms. At laparoscopy, the gall bladder was normal but the liver surface was noted to be studded with abscesses or metastases and a full laparotomy disclosed only the lesions diffusely on the surface of the liver. The patient remained febrile with leucocytosis and eosinophilia despite 2 weeks of post-operative antibiotics. The liver biopsy is shown in Image A and a CT scan of the liver taken 1 week post-operatively is shown in Image B.
|
|
Diagnosis: Fasciola hepatica infection, acute phase.
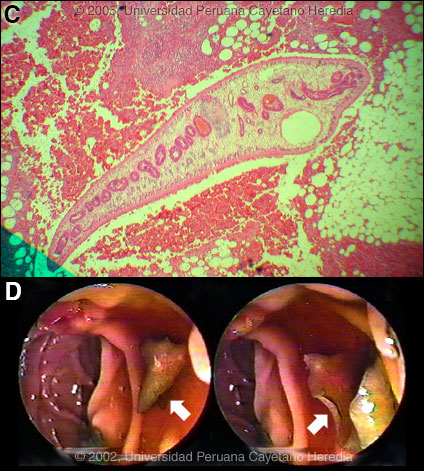
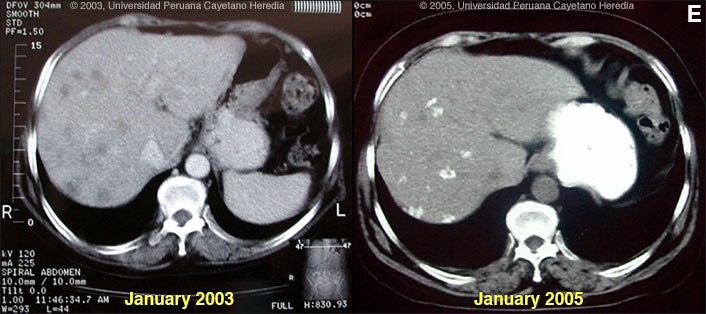
 Discussion: Further examination of omental tissue taken at the original surgery showed larvae of F. hepatica [Image C]. IgG FAS2 ELISA [Trans R Soc Trop Med Hyg. 1999 Jan-Feb;93(1):54-7] was positive for Fasciola hepatica at 3.2 OD units (Normal <0.2). Fasciola hepatica is a trematode (fluke or flatworm) in which the mature adult parasites inhabit the large biliary ducts. The adults are from 1 to 3 cm long and attach to the biliary epithelium by a single ventral sucker [Image D from our case files shows an endoscopic view of an adult in the common bile duct]. In the absence of direct visualization, characteristic eggs can be seen on stool examination, but more often patients present in the early migratory phases of infection prior to maturation of the worm and the onset of egg-laying. Specific serology is test of choice. As with all other trematodes, Fasciola hepatica requires a snail intermediate host. Eggs produced by the hermaphroditic adults pass with the feces and hatch, releasing larvae in fresh water. After passing through a snail, mature cercariae emerge and rapidly encyst on various kinds of aquatic vegetation such as watercress. After ingestion by a human or animal definitive host, the metacercariae excyst in the duodenum and larvae pentetrate the intestinal wall and subsequently migrate directly into the liver via Glisson's capsule. The larvae then embark on a destructive migratory process through the hepatic parenchyma for 3 to 4 months until they reach large biliary ducts where they mature to adults. The distribution of Fasciola hepatica is cosmopolitan, but is by far the most common in sheep-raising areas where herbivores are common definitive hosts. Heavily infected sheep develop "sheep liver rot". Other important definitive hosts are goats, cattle, horses, llamas, vicunas, and camels. The contiguous altiplano regions of the Peruvian and Bolivian Andes are highly endemic, with human prevalence rates of as high as 67% in some villages. Egypt, Cuba, and Northern Iran are also highly endemic. Cooking, which would kill the metacercariae, dramatically changes the flavor of watercress and the population is reluctant to adopt this simple measure. Our patient regularly ingested watercress. Clinically, the disease can be divided into acute and chronic phases. During the acute phase, migrating parenchymal larvae cause fever, eosinophilia, right upper quadrant pain and especially significant anorexia. Vomiting and weight loss of 20 kg or more may develop, which usually abates when the larvae mature to adults. The adult flukes in the biliary tree are generally asymptomatic but some patients develop chronic manifestations including right upper quadrant pain, nausea, vomiting, and hepatomegaly. Eosinophilia and abnormal liver function may develop but are less common than with acute disease. Adult flukes may cause hyperplasia, desquamation, thickening, and dilatation of the bile ducts. Malignant degeneration and cholangiocarcinoma such as results from chronic infection with the oriental liver fluke Clonorchis sinensis has not been reported with Fasciola hepatica. The differential diagnosis of hypereosinophilia with accompanying destructive hepatic lesions is limited. Toxocariasis causes hypereosinophilia with hepatomegaly but the pathology results from small granulomas around individual non-migrating larvae and not the large destructive tracks as was seen on the CT in our patient. Fasciola hepatica is the only trematode infection for which praziquantel is not the drug of choice. WHO has put the veterinary anthelmintic triclabendazole (Novartis) on its essential drugs list and has declared it the drug of choice despite the fact that human preparations are registered in only 2 countries. In Perú, the veterinary preparation is readily available and used. In the U.S. and many other countries the veterinary preparation can be obtained by special release from the manufacturer. The usual dosage is 10 mg/kg with a meal. Many practitioners repeat the dosage 12 to 24 hours later. In our institute the cure rate is 96% (A. Terashima, unpublished). Our patient was treated with a single 2-day cycle of triclabendazole 10 mg/kg/day with symptomatic improvement and no fever 2 weeks after treatment. WBC at follow-up was 7,800 with 20% eosinophils. Follow-up to Gorgas Case of the Week 2003-12 Only case reports but no series of sequential CT scans of the acute phase of fascioliasis have been published. Lesions are irregular, hypodense, sometimes oblong and branching. One recent published case shows serial CT scans over a 9-month period demonstrating changes in position, and shape of lesions over time, as would be consistent with the destructive nature of the migrating flukes [N Engl J Med. 2002 Apr 18;346(16):1232-9]. In a case seen by Gorgas participants in 2003 [Gorgas Case 2003-12] we demonstrated that in a case of massive fascioliasis, the destructive inflammatory tracks made by migrating larvae persist radiologically and histologically for months even after apparent parasitic cure. We have recently seen this patient in follow-up 2 years later and now report hepatic calcification as a sequelae of acute fascioliasis [Image E]. In addition, hepatic transaminases, alkaline phosphatase and bilirubin have been normal for the past 1 year, stool O & P remains negative, and the patient is asymptomatic. However, an eosinophilia of 8% persists.
 |