 |
Gorgas Case 2007-10 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. Each August we run one of our 2-week refresher courses for those with previous training in tropical medicine; currently running is the Gorgas Expert Course. For the past 7 years, we have been pleased to share interesting cases seen by the participants during the weeks of the year one of our courses is in session. Each case includes a brief history and digital images pertinent to the case. A link to the actual diagnosis and a brief discussion follow.
|
|
The following patient was seen in the inpatient department of the 36-bed Tropical Disease Unit at Cayetano Heredia National Hospital.
History: 21-year-old female patient first admitted 1 year earlier with painless papular lesions and a violaceous plaque on the right knee that that had been progressive over 4 years after trauma to that area. The patient had initially received empiric therapy over the years with oral fluconazole for approximately 45 days and then clarithromycin plus cotrimoxazole for 8 months with no improvement. A new papular lesion on the left thigh that evolved to a violaceous plaque developed 4 months prior to that admission. After a biopsy diagnosis was made, the lesions improved with 3 weeks of parenteral followed by continuous oral antimicrobial therapy. The patient was readmitted 3 months ago with a 2-month history of reactivation of the previous lesion on the left thigh, and the appearance of 2 new small papular lesions, 1 on the left breast and 1 on the dorsal chest area. No fever, chills, weight loss, or cough. Headache with no other neurologic complaints have developed during the current hospitalization. Epidemiology: The patient was born in Lima and lives in Lima. No history of travel to the jungle. There is no history of exposure to TB, no specific occupational exposures, and no history of swimming in brackish or contaminated fresh or sea water. Physical Examination: (on re-admission). Afebrile. Chest clear. No hepatosplenomegaly. Normal CNS exam. Skin lesion at initial admission is shown in Image A and at the beginning of the current re-admission in Image B. Laboratory Tests: (on re-admission). Hct 30, normal WBC with no eosinophilia. Normal liver function. Normal Chest X-ray. HIV and HTLV-1 negative. MRI is shown in Images C & D. A CT scan obtained elsewhere 4 months earlier was reported as normal. CSF contained 2 WBC (100% lymphs) with normal glucose and proteins and all stains were negative. 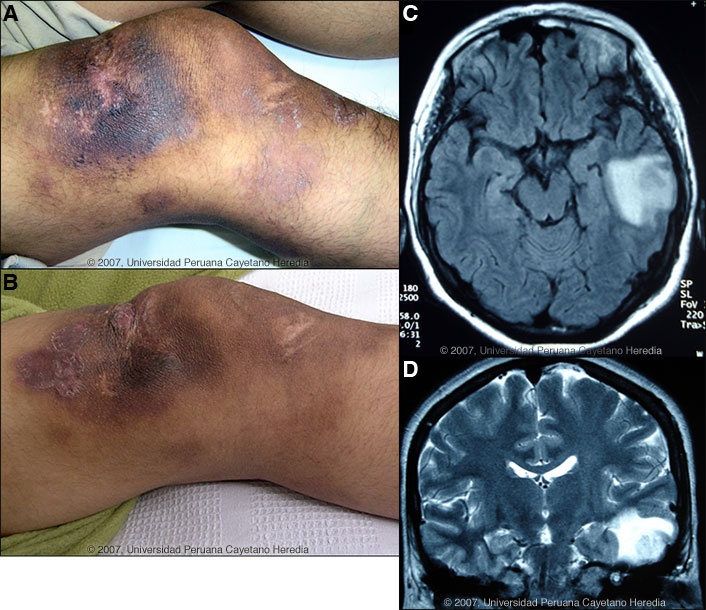
 |
|
Diagnosis: Balamuthia mandrillaris (free-living amoeba) responsive to miltefosine.
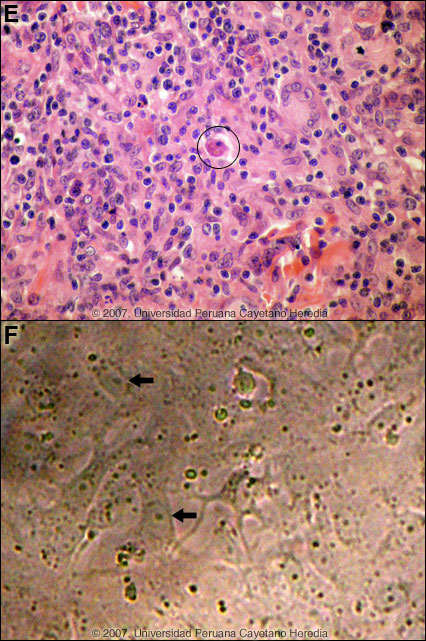
 Discussion: A biopsy of the lesion on the right knee was performed at the intial admission [Image E]. A dense inflammatory infiltrate of the dermis composed of lymphocytes, plasma cells and multinucleated cells with granulomas is seen. A trophozoite of a free-living amoeba with a small eccentrically located nucleus and vacuolated cytoplasm is shown in the circle. In addition, B. mandrillaris was isolated in culture from the skin [Image F, arrows]. Isolation of B. mandrillaris requires the use of Vero cells at 37°C with 5% CO2. Lysis of the cells signals the presence of the ameba, which was confirmed as B. mandrillaris by PCR both at our institution and at the Public Health Department of California. However, other species of free-living ameba are not known to occur in Perú. A sample from the backyard of her house was cultured and was also positive. Around 100 cases of Balamuthia mandrillaris have been reported since the organism's initial description in 1990 [Clin Infect Dis. 1997 Dec;25(6):1354-8]. Half or so have been in the USA, mostly in immunocompromised patients. Cases have also occurred in Canada, Mexico, Australia, Argentina, Brazil, Mexico, Thailand, Japan, the Czech Republic, Portugal, and England. A significant number of the published cases from the United States have occurred in persons of Hispanic ethnicity. Additional reports have come from Canada, Japan, Australia, Thailand, and Eastern Europe, as well as from throughout Latin America. We have seen over 50 cases at our institution and, like most Latin American cases, the patient is not immunocompromised. Unlike Acanthamoeba and Naegleria species, which are more familiar to clinicians and known to occur in brackish ponds and creeks, an ecologic niche in nature has not been definitively found for Balamuthia. Our patients have come from throughout Perú, and usually, but not always, have a history of swimming in potentially contaminated fresh water. Entry of water into the nasal mucosa and the olfactory nerve endings is thought to occur with Acanthamoeba and Naegleria. Naegleria infection causes an acute necrotizing and suppurative meningoencephalitis, an aggressive disease that is generally fatal in days. Acanthamoeba cause a sub-acute granulomatis encephalitis with a more prolonged but ultimately fatal course. Occasionally patients with Acanthamoeba have a skin lesion usually described as a chronic ulcer. Acanthamoeba, unlike Balamuthia, has been associated also with amoebic keratitis, a painful sight-threatening disease of the eye. In Balamuthia infection the disease may follow a prolonged course, but most frequently has a fatal outcome. Almost all cases have an initial skin lesion, and this lesion precedes the inevitable CNS disease (granulomatous amebic encephalitis) by weeks or months. Patients have ranged from 5 to 65 years of age with 50% under age 15. The typical skin lesion is a single painless plaque up to several centimeters in diameter; a few patients have had 2-3 lesions. Color may be skin tone, dark red, or slightly violaceous. Sensation is preserved. Location is usually on the central face, so that this patient represents the fewer than 10% with inicial lesions on trunk or extremities. For facial lesions the differential diagnosis may include tuberculosis, mucocutaneous leishmaniasis, leprosy, sporotrichosis, paracoccidioidomycosis, rhinoscleroma, or mucormycosis. Sarcoid, discoid lupus, and Wegeners can also be considered. Histologically, granulomatous inflammation with lymphocytes, histiocytes, plasma cells, as well as giant cells, is characteristic. Amoebic trophozoites are often scanty and multiple sections need to be examined. Some foci of vasculitis may be present. CNS involvement most often manifests with heachache, photophobia, seizures that progress to lethargy, sensori-motor deficit, coma and death. The CNS lesion is a progressive hemorrhagic necrosis with large numbers of amoebic trophozoites and cysts invading vascular sub-adventitial areas of arteries, veins, and capillaries, leading to perivasculitis and cerebral infarcts [Hum Pathol. 1999 Mar;30(3):269-73]. No therapy has been shown to be highly effective in curing Balamuthia infection. With IV amphotericin B or pentamidine, an initial and apparently favorable response or disappearance of cutaneous lesions still does not halt the eventual appearance of CNS disease. Similarly, in our hands, multi-drug combination therapy with agents such as albendazole, itraconazole, or fluconazole have still resulted in eventual appearance or progression of CNS disease. In our hands there have been 5 survivors out of 11 patients treated with aggressive combination therapy followed by 6-12 months of albendazole maintenance. One or two case reports from other centers have reported success with regimens that have also included sulfadiazine, macrolides and phenothiazines. At the initial admission the current patient was started on amphotericin B (0.7 mg/kg/d) + itraconazole (200 mg/d) + albendazole (400 mg/d) until completing 1.5 gm of amphotericin B. She was then discharged on oral therapy only after a significant improvement of both lesions. A surgical resection of the left thigh lesion was performed, and oral cotrimoxazole was added. On re-admission 3 months ago for the reactivation, amphotericin B was added to the oral regimen of itraconazole, albendazole and cotrimoxazole with no improvement resulting after a further one month of therapy. Clarithromycin (1500 mg/d) and oral artesunate (100 mg/d) were added, and itraconazole was replaced with fluconazole (450 mg/d). 
 Miltefosine is now established as effective anti-leishmanial therapy. A recent report showing good in vitro activity of miltefosine against Balamuthia, Acanthameba, and Naegleria [J Eukaryot Microbiol. 2006 Mar-Apr;53(2):121-6] led us to commence Miltefosine (150 mg/d for 12 days, then 100 mg/d chronically thereafter) and clarithromycin-cotrimoxazole-artesunate and amphotericin B were stopped as no clinical improvement was observed. After 37 days of miltefosine therapy, Image G shows partial healing of the skin lesions and the MRIs in Images H & I demonstrate significant improvement in the CNS lesion. The patient remains on miltefosine, fluconazole and albendazole. Unlike the patient we presented earlier this year [Gorgas Case 2007-06] who died rapidly after appearance of CNS disease, this patient has at least a short-term response to therapy. 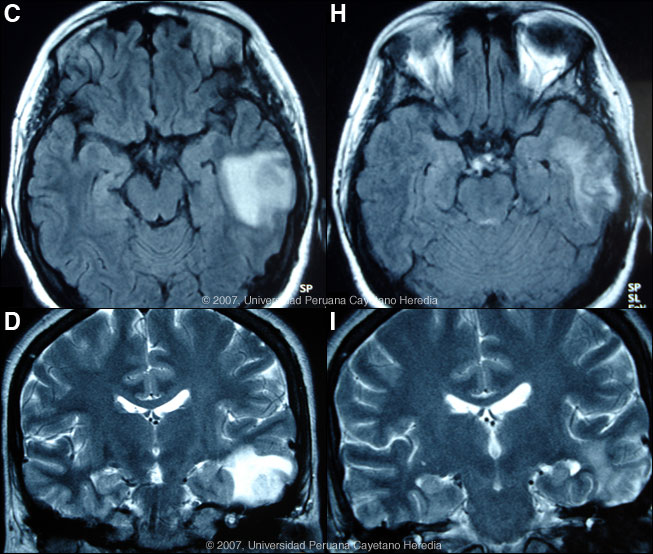
 |