2009 Case #10 |
 |
| Diagnosis: Paracoccidioidomycosis due to Paracoccidioides brasiliensis. |
|
Intestinal involvement in paracoccidioidomycosis is uncommon with only case reports [Gut. 1979 Oct;20(10):896-9.] and discussion as a complication in all comprehensive reviews from Brazil, the major endemic area [Dermatol Clin. 2008 Apr;26(2):257-69, vii. Review.]. No systematic studies include GI complications. Route of acquisition may be either inhalation or ingestion of organisms; conclusive data is not available. The major differential diagnosis in Perú of colonic ulcers would include amebiasis, TB, and Balantidium coli [Gorgas Case 2002-07]. Ulcers due to typhoid fever are usually in the ileum or proximal colon and would be preceded by a progressive febrile illness over weeks without diarrhea [Gorgas Case 2009-04]. The chronic form of paracoccidioidomycosis most often involves pulmonary disease with oral mucosal involvement as a frequent complication [Gorgas Case 2004-05]. The differential diagnosis for the lung disease includes: TB, histoplasmosis, lymphoma, cancer and cryptococcosis. Although the pulmonary involvement is mild in this patient, she demonstrates the most typical radiographic pattern of paracoccidioidomycosis with bilateral mixed infiltrates (alveolar and interstitial), mainly located in the middle and lower lobes. Interstitial lesions may have miliary, nodular or fibronodular patterns. Other patterns observed in these patients are hilar and mediastinal lymph node enlargement, cavities, and calcified lesions. Extrapulmonary disease is found in over 70% of cases and may involve skin, mucous membranes, lymph nodes, adrenals, abdominal organs and CNS (in 9-25%). In our experience the male:female ratio in chronic paracoccidioidomycosis is 20:1, as generally it is males that have the most extensive occupational exposures in rain forested areas of South America. Paracoccidioidomycosis, also known as South American blastomycosis, is found in humid forested or lush green areas of the Americas from Southern Mexico south to Uruguay and Argentina. It appears to be most common in Brazil. The exact habitat of the organism is unclear but transmission is most often described as being entirely by airborne inhalation. Travelers spending less than 6 months in an endemic area are unlikely to acquire paracoccidioidomycosis. Sulfonamides, ketoconazole, itraconazole, and amphotericin B are all effective therapies. Amphotericin should be reserved for severe cases such as this one. For typical cases, itraconazole 100-200 mg/day for 6-9 months is regarded as the treatment of choice when it is available and affordable. Relapses are common with less than 6 months therapy and expert opinion is now that 1 year is not necessary. In the developing-world setting, ketoconazole is likely equally effective and is usually less than half the cost. However, 12 months of therapy with ketoconazole is generally recommended. In severe cases with a high yeast burden, such as in our case, the practice is to induce such patients with amphotericin B for at least 10 days at up to 1 mg/kg, then switch to oral itraconazole 200 mg per day, to complete a total duration of at least 9 months. This patient was started on amphotericin B. On the tenth day of treatment she had a generalized seizure that was followed 24 hours later by amaurosis and left side hemiparesis, with complete recovery in about 24 hours. An MRI disclosed hypodense lesions in the right frontal and parietal lobes on the T1 images and intense signal on the T2 and FLAIR images [Image E]. CSF examination showed: no leukocytes, glucose 60 mg/dl, protein 13 mg/dl (all normal), opening pressure was normal. CNS involvement occurs between 9-25% of cases [Braz J Infect Dis. 2005 Apr;9(2):126-33. Review.]. Focal lesions with enhancement are the most common manifestations; meningitis has also been reported. CSF findings show elevation of proteins with no cells and normal glucose in these patients with focal neurological findings; the culture is usually negative. In up to one-third of these cases the CNS manifestations occur late in the disease course and well after any other clinical manifestations. Our patient has multiple ischemic lesions that have apparently not been reported before. |
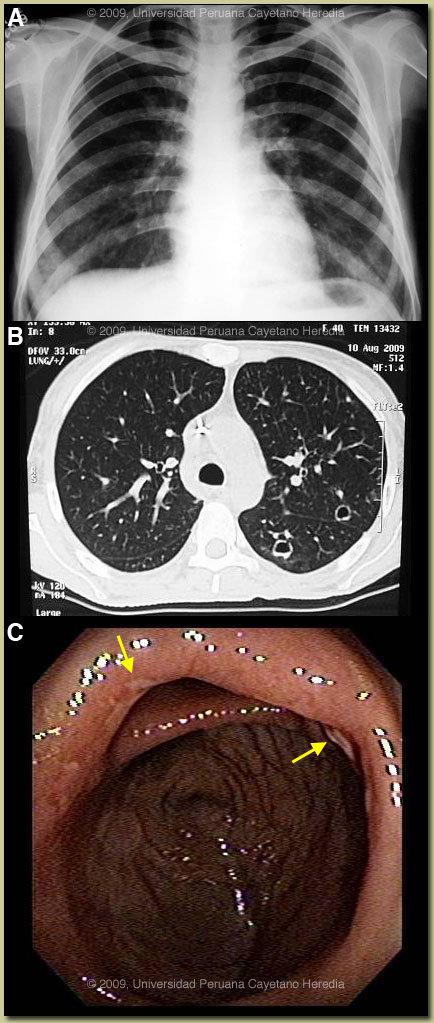
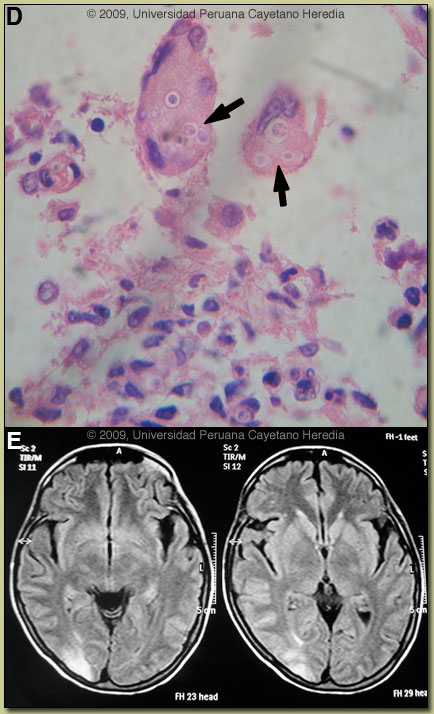 Discussion: A biopsy of a colonic ulcer disclosed a dense chronic inflammatory reaction with granuloma formation and intracellular yeast forms within multinucleated giant cells [Image D, arrows]. No cultures were done at the time of biopsy but subsequent stool culture (+) for P. braziliensis. Further work-up of the lung lesion is pending. HTLV-1 (+); no association between HTLV-1 and paracoccidioidomycosis has been reported despite both agents being common in many areas of Brazil.
Discussion: A biopsy of a colonic ulcer disclosed a dense chronic inflammatory reaction with granuloma formation and intracellular yeast forms within multinucleated giant cells [Image D, arrows]. No cultures were done at the time of biopsy but subsequent stool culture (+) for P. braziliensis. Further work-up of the lung lesion is pending. HTLV-1 (+); no association between HTLV-1 and paracoccidioidomycosis has been reported despite both agents being common in many areas of Brazil.