2011 Case #2 |
 |
| The following patient was seen in the inpatient department of the 36-bed Tropical Disease Unit at Cayetano Heredia National Hospital. |
|
Epidemiology: Farmer from the jungle. Physical Examination: HR 88, RR 18, BP 100/60. Afebrile. Painful ulcerated lesions on all limbs [Images A, B], a single abdominal wall lesion, and nodular lesions on the arms [Image C]. Chest clear, no mucosal lesions, no lymphadenopathy, no hepatosplenomegaly. Laboratory: Hb 10. WBC 8900 (56 polys, 10 lymphs). CXR normal. Stool O & P negative. Normal hepatic and renal function. |
| Diagnosis: Disseminated sporotrichosis. |
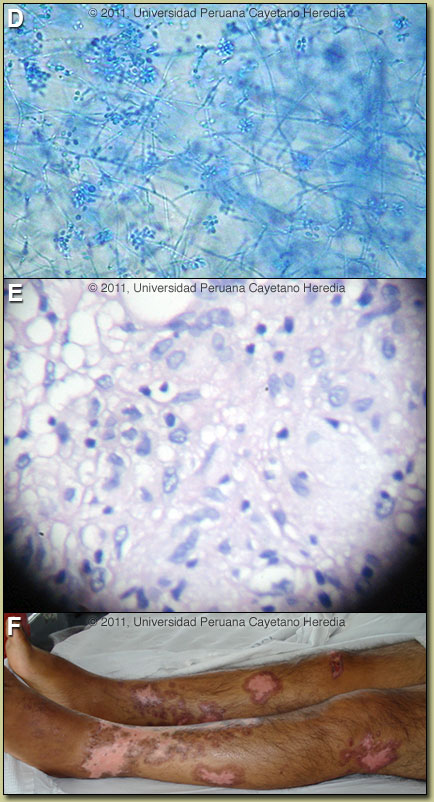 Discussion: Sporotrix schenkii was cultured [Image D] from a skin biopsy which showed histiocytes and lymphocytes without well formed granulomas [Image E]. In culture of aspirates or biopsy material, S. schenkii grows very easily and rapidly when present. Smears or aspirates from the lesion are usually negative on direct examination and no useful serology is available. AFB, Giemsa, and PAS stains of the tissue were negative. Cutaneous leishmaniasis had been suspected earlier in the illness and a course of presumptive antimonials was without effect. Discussion: Sporotrix schenkii was cultured [Image D] from a skin biopsy which showed histiocytes and lymphocytes without well formed granulomas [Image E]. In culture of aspirates or biopsy material, S. schenkii grows very easily and rapidly when present. Smears or aspirates from the lesion are usually negative on direct examination and no useful serology is available. AFB, Giemsa, and PAS stains of the tissue were negative. Cutaneous leishmaniasis had been suspected earlier in the illness and a course of presumptive antimonials was without effect.
The differential diagnosis of disseminated nodular and ulcerated lesion in Perú includes leishmaniasis, sporotrichosis, atypical mycobacteria, and nocardiosis. Sporotrichosis is always an important consideration in areas such as Perú even where leishmaniasis is much more common. In normal hosts linear sporotrichoid lesions on an extremity would be the most common presentation of sporotrichosis [see Gorgas Case 2008-01]. In normal hosts, extracutaneous manifestations of sporotrichosis include osteoarticular, meningeal, and pulmonary sporotrichosis. These are usually seen in immunocompromised hosts and in alcoholics. In the last 2 decades a systemic presentation restricted almost exclusively to HIV patients has been described [Curr Fungal Infect Rep. 2011;5(1):42-8]. Environmental reservoirs for S. schenkii include sphagnum moss (including wood or plants contaminated by moss), decaying vegetation, hay, soil and masonry. Outdoor work including farming, construction, gardening, and having a cat are risk factors [Clin Infect Dis. 2004;38(4):529-35 and Clin Infect Dis. 2003;36(1):34-9]. Acquisition is generally by local inoculation, but in disseminated cases like this inhalation followed by hematogenous dissemination cannot be ruled out. Sporotrichosis is distributed worldwide but most cases are reported from the Americas and Japan. Most cases are sporadic or occur in self-limited clusters due to some point source exposure. The area around Abancay, Perú (not where this patient lives) has recently been, perhaps uniquely, identified as an area where sporotrichosis is not only entrenched but is hyperendemic with annual incidence rates of up to 100 per 100,000 population [Clin Infect Dis. 2003;36(1):34-9 and Clin Infect Dis. 2000;30(1):65-70]. Guidelines for treatment of sporotrichosis have been released by the Infectious Diseases Society of America [Clin Infect Dis. 2007;45(10):1255-65] and are partly based on work from our Institute. The treatment of choice for lymphocutaneous sporotrichosis is itraconazole and in severe extracutaneous or disseminated disease amphotericin can be used. Terbinafine has been shown to be effective therapy [Mycoses 2004;47(1-2):62-8]. Posaconazole has good in vitro activity but voriconazole and ravuconazole are not active in vitro against S. schenckii. Fluconazole is ineffective against sporotrichosis. There are no published trials or series for therapy of disseminated disease in AIDS patients. Most do poorly no matter the regimen. Our patient was treated with Amphotericin B for 8 weeks and then itraconazole is being used to complete a minimum of 1 year. ART was changed to AZT, 3TC, lopinavir/ritonavir because of itraconazole interactions with nevirapine. Follow up at 2 months showed marked improvement [Image F]. |
 History: 38 year old with HIV and culture positive MTb from a cervical lymph node diagnosed 6 months earlier. Approximately 7 months prior to admission he developed fever, painless nodular lesions on both arms, as well as cervical adenopathy. The fever and adenopathy subsided on 4-drug TB therapy but the cutaneous lesions ulcerated and new lesions developed and became confluent. Because of a CD4 of 70, ART (AZT, 3TC, NVP) was commenced 4 months prior to admission.
History: 38 year old with HIV and culture positive MTb from a cervical lymph node diagnosed 6 months earlier. Approximately 7 months prior to admission he developed fever, painless nodular lesions on both arms, as well as cervical adenopathy. The fever and adenopathy subsided on 4-drug TB therapy but the cutaneous lesions ulcerated and new lesions developed and became confluent. Because of a CD4 of 70, ART (AZT, 3TC, NVP) was commenced 4 months prior to admission.