 |
Gorgas Case 2008-01 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. For the eighth consecutive year, we are pleased to share interesting cases seen by the participants that week during the February/March course offerings. Presently the 9-week Gorgas Course in Clinical Tropical Medicine is in session. New cases will be e-mailed every Monday for the next nine weeks. Each case includes a brief history and digital images pertinent to the case. A link to the actual diagnosis and a brief discussion follow.
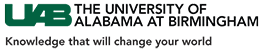
The following patient was seen in the outpatient department of the 36-bed Tropical Disease Unit at Cayetano Heredia National Hospital. 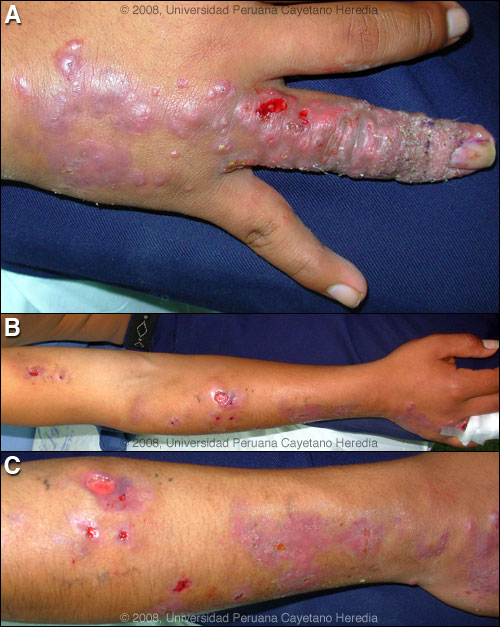 History: 21 year-old male with painless skin lesions restricted to the right arm. The initial lesion began from the base of the nail of the 4th finger 3 months earlier that progressed to multiple non-pruritic popular and ulcerative lesions which have continued to spread and progress. Some nodules ulcerated with a clear yellowish discharge. No history of fever, general malaise, weight loss or any constitutional symptom. No specific recollection of any traumatic lesion. Epidemiology: Patient was born and lives in the highlands of Cajamarca. He works as a corn farmer, but also raises cattle, chicken, guinea pigs and dogs. No ill contacts, no relevant family history, no TB contact. Physical Examination: Afebrile. Physical examination normal except for right arm as shown in Images A-C. Right epithroclear but not axillary lymphadenopathy. Laboratory Examination: Normal Chest X-ray. Specimens from the lesions were sent for stain, culture and histology.
|
|
Diagnosis: Sporotrichosis.
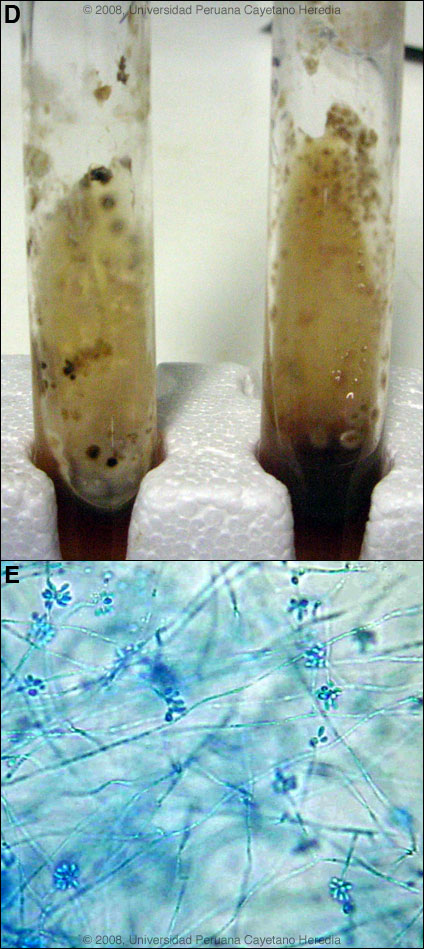 Discussion: Scrapings from the site of the intial lesion at the base of the nail were cultured on Sabouraud’s agar and yielded characteristic colonies on the slant [Image D] after 3 days of culture at 30°C. Hyphae and the characteristic bouquet-like conidia of Sporothrix schenkii were seen microscopically [Image E]. In culture of aspirates or biopsy material, S. schenkii grows very easily and rapidly when present. Smears or aspirates from the lesion are usually negative on direct examination and no useful serology is available. An aspirate, scrapings and biopsy from an arm ulcer were negative for leishmaniasis by culture in NNN media, PCR, and direct examination. Histopathology was negative for leishmania. A leishmanin skin test was negative. The differential diagnosis of an ulcerated lesion with linear lymphocutaneous spread in Perú includes leishmaniasis, sporotrichosis, atypical mycobacteria, and nocardiosis. Sporotrichosis is always an important consideration in areas such as Perú even where leishmaniasis is much more common. It is not possible purely on clinical grounds to differentiate the two with certainty. Our leishmania referral clinic sees hundreds of cases a year and fungal cultures are routinely performed. S. schenkii is a dimorphic fungus but the oval to cigar shaped yeast forms are difficult to find on biopsy specimens. Cutaneous anthrax occurs in Perú [see Gorgas Case 2001-07] and can have lymphatic spread but a lesion of this duration would consistently have a black necrotic base. Loxocelism often evolves to a large ulcer but those lesions are uniformly extremely painful unlike in the current case. Environmental reservoirs for S. schenkii include sphagnum moss (including wood or plants contaminated by moss), decaying vegetation, hay, soil and masonry. Outdoor work including farming, construction, gardening, and having a cat [Clin Infect Dis 2004;38(4):529-35 and Clin Infect Dis 2003;36(1):34-9] are risk factors. Sporotrichosis is distributed worldwide but most cases are reported from the Americas and Japan. Most cases are sporadic or occur in self-limited clusters due to some point source exposure. The area around Abancay, Perú (not where this patient lives) has recently been, perhaps uniquely, identified as an area where sporotrichosis is not only entrenched but is hyperendemic with annual incidence rates of up to 100 per 100,000 population [Clin Infect Dis 2003;36(1):34-9 and Clin Infect Dis 2000;30(1):65-70]. Extracutaneous manifestations of sporotrichosis include disseminated visceral, osteoarticular, meningeal, and pulmonary sporotrichosis. These are usually seen in immunocompromised hosts and in alcoholics. These manifestations are rare or even unknown in Perú. New guidelines for treatment of sporotrichosis have recently been released by the Infectious Diseases Society of America [Clin Infect Dis 2007;45(10):1255-65] and are partly based on work from our institute. The treatment of choice for lymphocutaneous sporotrichosis is itraconazole and in severe extracutaneous or disseminated disease amphotericin can be used. Terbinafine has been shown to be effective therapy [Mycoses 2004;47(1-2):62-8]. In the reality of poor countries, many patients cannot afford itraconazole or terbinafine. The older but still effective mode of therapy with a saturated solution of potassium iodide (SSKI) is still widely used in practice. However, our patient has been started on itraconazole. SSKI and its clinical use has been recently reviewed [J Am Acad Dermatol 2000;43(4):691-7] and we have previously demonstrated the utility of once daily dosing in order to increase compliance [Pediatr Infect Dis J 1996;15(4):352-4]. The mechanism of action is unknown. SSKI can also be used for entomophthoramycosis caused by Basidiobolus and Conidiobolus. In dermatologic practice SSKI can be used for erythema nodosum, nodular vasculitis, erythema multiforme, and Sweet’s disease. The main adverse effects are gastrointestinal and the SSKI can be added to larger volumes of water, juice, or milk for administration. Care must be taken to avoid potassium or iodide toxicity in those on ACE inhibitors or potassium sparing diuretics, those with renal disease, and in those on medications or with conditions making them unable to autoregulate thyroid hormone production. There are no published data regarding the new azoles, voriconazole and posaconazole. Voriconazole is not active in vitro against S. schenckii, whereas posaconazole does have activity in vitro. Fluconazole is ineffective again sporotrichosis.
|