 |
Gorgas Case 2015-01 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. For the 15th consecutive year, we are pleased to share interesting cases seen by the participants that week during the February/March course offerings. Presently the 9-week Gorgas Course in Clinical Tropical Medicine is in session. New cases will be sent by e-mail every Tuesday/Wednesday for the next 9 weeks. Each case includes a brief history and digital images pertinent to the case. A link to the actual diagnosis and a brief discussion follow.
David O. Freedman & Eduardo Gotuzzo
Course Directors |
|
The following patient was seen on the wards of the 450-bed Cayetano Heredia National Hospital in Lima, Perú.

 History: 61-year-old female patient presented to the Emergency Department with a 5-day history of acute pain and discoloration of the left arm. While carrying a piece of wood she suddenly felt a sharp stabbing pain in her upper arm, and 3 hours later she noticed an initial erythematous lesion and swelling. The pain persisted and 1 day later she noticed having dark urine. One day prior to admission she noted nausea and vomiting without hematemesis. Lesions and discoloration continued to spread over the 5 days. She denies sweating, abdominal pain, fever, headache, neurologic deficit or changes in urinary volume.
Epidemiology: Housewife, born and currently living in Cañete (southern coastal area of Lima Department). No history of travel. Physical Examination: HR: 60; RR: 20; BP: 130/60; Temp: afebrile. Skin: pallor, no jaundice. Examination of the left arm on Day 15 of illness is shown in Image A. The arrow denotes an initial 1 cm area of what had been a blister on the proximal arm that became necrotic with 2 other similar lesions distally [arrow with N]. An area of purple discoloration centrally with a spreading area of white vasoconstriction and a red vasodilated erythematous halo was also present. Laboratory Examination (on admission): BUN 226 mg/dl, creatinine 5.7 mg/dl, Hb 10.6 mg/dl; WBC 8.0 with normal differential; platelets 160,000. INR 1.14. Glucose 126 mg/dl, Na 136, K 6.2, Cl 104. AST 50 mg/dl (<40), ALT 98 mg/dl (<40), Alk Phosphatase and GGT normal. Total bilirubin 1.0 mg/dl (conjugated 0.4 mg/dl, unconjugated 0.6 mg/dl), LDH 2,276 U/l (<140); CK 178 U/l (<176); pH 7.37, pO2 90.2, pCO2 32.0, HCO3 18.9. Urinary sediment: RBC 70-80/hpf, WBC 0-6/hpf.
|
|
Diagnosis: Necrotic arachnidism due to bite of the South American brown recluse spider Loxosceles laeta [shown in Image B].
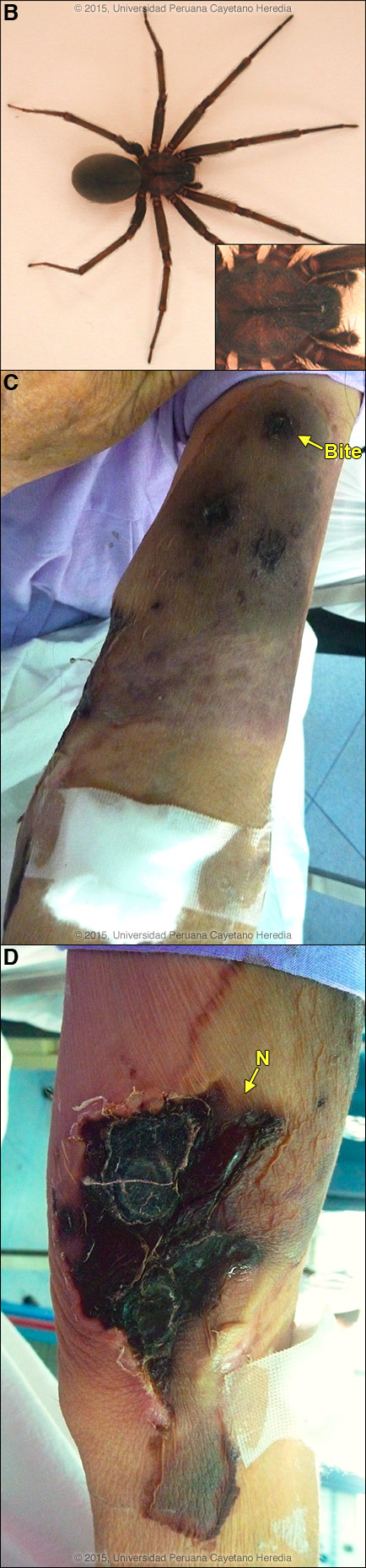
 Discussion: The diagnosis of loxoscelism is a clinical one though definitive criteria for the diagnosis require knowledgeable species identification of the offending spider. In this case, the patient had not seen or captured the spider. L. laeta are highly prevalent throughout much of Lima. The spectrum of disease ranges from a mild skin irritation, to severe local necrotic reactions, to a less common syndrome (10-15% of cases), as in this patient, of viscerocutaneous loxoscelism manifested with vasoconstrictive blanching, sometimes a dengue-like scarlatiniform rash, hemolysis and renal failure. Mortality may uncommonly occur in severe cases and is higher in children due to lower body weight per amount of venom injected. The classic “red, white and blue” sign is virtually diagnostic as the lesion evolves. The erythematous outer ring is vasodilatation, the middle white ring is vasoconstriction, and the central blue is pre-necrotic cyanosis early followed by actual necrosis. Other examples from our files include Gorgas Cases 2008-03 and 2003-08. The patient often notes the initial bite, but it usually takes several hours for the onset of severe pain as the venom spreads. The violaceous central plaque represents an area of hemorrhage and thrombosis, which in more severe cases will progress to frank necrosis. The bite of Loxosceles laeta is thought to cause more extensive and severe necrosis when compared to the related and well-studied brown recluse spider Loxosceles reclusa found in the United States. When the lesions do evolve there is a hemorrhagic bulla, ulceration, and development of necrotic centers. The borders are irregular, influenced by gravitational factors (well shown here) as venom spreads in a manner related to the body part affected, and without significant surrounding edema. At least 54 species of Loxosceles are described from North and Central America and 30 species from South America, and additional species are found in Africa and the Mediterranean. Loxosceles laeta is native to Perú, Chile, Ecuador, Argentina, Uruguay, and south and eastern Brazil. It has been accidentally introduced into the U.S. and several Central American countries at various times but does not naturally thrive in those locations. Loxosceles laeta is similar in appearance to other recluse spiders but is generally larger with a body length up to 15 mm. The head region has dark violin shaped markings on the dorsal aspect [Image B inset] but these markings cannot be reliably used to identify recluses as other types of spiders may have similar markings. Loxosceles laeta accounts for 98% of loxosceles cases in Perú, but is only seen in coastal regions and up to 1,200 m in the Andes and never in the jungle regions. However, jungle species such as L. amazonica may be found in Brazil. They live most commonly in very domestic environments in both urban and rural areas, often hiding in clothing in drawers or in closets. They are not aggressive and only bite when disturbed or threatened. Bites occur more commonly in summer (January to April) when the spider reproduces and most bites occur at night or in the early morning. Polyclonal equine IV antiserum produced in Brazil is sometimes available in Perú but is not widely used. Work in animal models has shown anti-venom to be effective if administered in the first 12 to 24 hours after a bite, but prospective controlled human clinical trials are lacking in any country [Toxicon. 2006 Aug;48(2):123-37]. Retrospective data is limited by lack of definition of time to antivenom administration and relation of that parameter to outcome. Our patient presented 5 days after the bite so antivenom was not considered. There is no commercial product available in North America. In Perú, as in many other countries that have various Loxosceles species, dapsone is sometimes administered at 100 mg/day for 1 week unless patients already have active hemolysis (excluding our patient) or are G6PD deficient. No controlled trials have been reported; the practice is controversial, but clinical experience in Perú and several limited studies support this practice. G6PD deficiency does not occur in Perú. Systemic corticosteroids are often considered but again, no clinical trials support the practice. Patients such as ours with any evidence of hemolysis or hemoglobinuria require vigorous intravenous hydration and urinary alkalinization. Aggressive debridement and escharectomy is advised but only once the acute phase is over; debridement too early may increase tissue loss. As per protocol our patient was put on clindamycin in case of bacterial superinfection. Renal function continued to deteriorate and the patient received 4 sessions of hemodialysis with eventual resolution of serum Cr to 2.3 on Day 17 after the bite. On Day 19 necrosis was continuing to progress (Image C shows the original bite site proximally, and N in Image D corresponds to the same area as shown earlier in Image A). Surgical scar revision will eventually be performed after the progression of the necrosis ceases.
|