 |
Gorgas Case 2016-10 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. Each August we conduct one of our 2-week refresher courses for those with previous training in tropical medicine; currently in session is the Gorgas Advanced Course. There will be one more case next week to complete the 2016 case series.
The following patient was seen by the Gorgas Advanced Course participants in the outpatient clinic of the Tropical Medicine Institute in Lima. Eduardo Gotuzzo and German Henostroza Course Directors 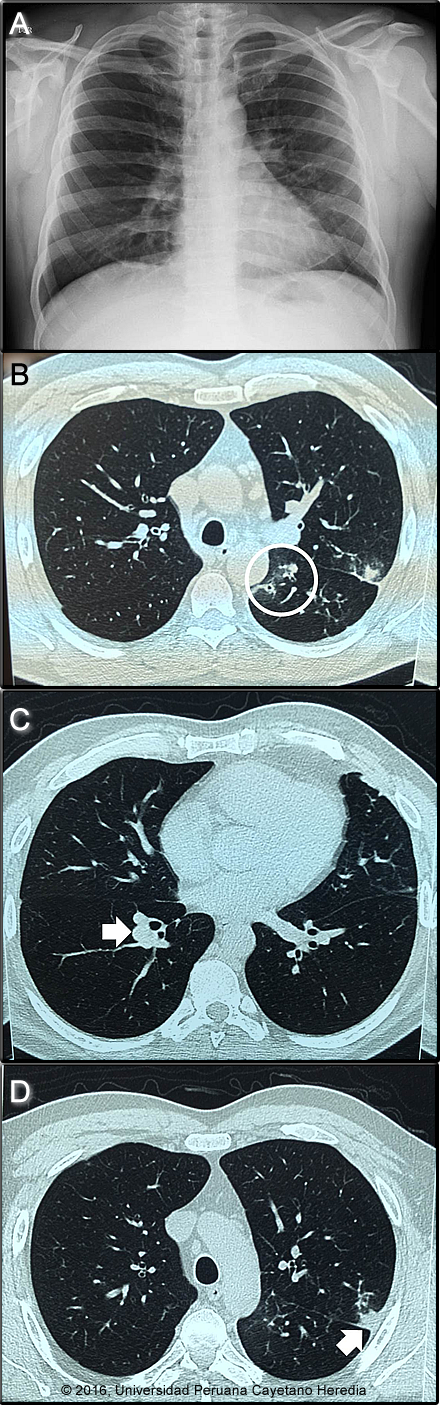
 History: 41 year-old previously healthy male presented with a 2-year history of persistent cough and blood-tinged sputum. Some episodic hoarseness that started shortly after cough onset responded to antibiotics but sputum production persisted. Three months before presentation an episode of hemoptysis of a half teaspoon of clotted blood heralded the onset of left anterolateral chest pain, especially when coughing. He denies fever, weight loss, sweating or shortness of breath. Chest x-ray, chest CT, and bronchoscopy prior to referral showed left lower lobe consolidation with pleural thickening. Repeated AFB stains and microbiological examinations were reported as negative.
Epidemiology: Born and had lived for 25 years in Chilete, on the Jequetepeque River in Cajamarca in Northern Peru. A schoolteacher, he currently lives in San Pablo with his wife and two children but returns to his hometown every weekend and drinks heavily. Denies tobacco or recreational drug use. No known TB contacts. He travels frequently within the provinces of Cajamarca. Physical Examination: HR 74. RR 18. BP 110/70. Afebrile Healthy appearing and alert. HEENT: nasopharynx clear, no cervical adenopathy. Chest: Clear breath sounds to auscultation bilaterally. Cardiovascular: Regular rate and rhythm, S1/S2 normal, no murmurs. Abdomen: normal bowel sounds, soft, non-tender, non-distended. No hepatosplenomegaly. Skin and extremities: no rash, nodules, no edema. Laboratory Examination (on admission): WBC 6.18 (0 bands 50 neutrophils, 10 eosinophils, 3 monos, 37 lymphs). Hb 14.8 g/dL, Hct 44%. Platelets 194 000. Glucose, urea, creatinine normal. Chest X-ray and Chest CT are shown (Images A-D). Bronchoscopy showed chronic inflammation of the bronchial tree with bronchiectasis and spontaneous, self-limited bleeding. Bronchial aspirate: gram stain showed few Gram positive cocci with 1-3 WBC per hpf and negative culture; negative AFB;: negative KOH and fungal culture. Pap was negative for malignant cells. Stool O&P: Blastocystis sp. 2-4/hpf, Endolimax nana 2-4/hpf.
UPCH Case Editors: Carlos Seas, Clinical Course Coordinator/Sofia Zavala, Associate Coordinator UAB Case Editor: David O. Freedman, Course Director Emeritus |
|
Diagnosis: Pulmonary paragonimiasis due to P. mexicanus

 Discussion: After multiple negative tests, a sputum processed and examined for ova and parasites demonstrated eggs of the lung fluke Paragonimus sp. [Image E]. Ova are often swallowed and found in stools but all stool exams were negative in our patient. On further questioning the patient admitted to catching and eating uncooked fish and fresh-water crab ceviche on his weekends. The radiologic images were read as showing, right apical pleural thickening (Image A), and the CT showing a right peribronchial nodule, left subpleural nodular lesion with cavitation, and some ground glass opacities. In paragonimiasis, typical chest x-ray findings include focal or segmental air-space consolidation, cystic lesions, linear opacities or pleural effusion. The cavities may be multilocular. The most frequent CT finding is a poorly marginated subpleural or subfissural nodule of 2 cm in diameter containing a low-attenuation area, associated with pleural thickening. These lesions are commonly found in the mid and lower lung zones, as opposed to the upper lobes in tuberculosis. Pulmonary nodules and hemoptysis are not only caused by TB in highly endemic areas. Differential diagnosis in cases such as these include: paragonimiasis, dirofilariasis, nocardiosis, aspergilloma, endemic fungal diseases such as cryptococcosis, coccidiodomycosis and histoplasmosis, and cancer. Paragonimiasis is a zoonoses caused by infection with lung flukes (trematodes) of various species. In Asia, the infection is most prevalent in China, Korea, Japan, Taiwan, the Philippines, and Thailand, with Paragonimus westermani the most common species. Other Asian species infecting humans include P. skrjabini, P. miyazakii, and P heterotremus. Infection in West Africa is due to P. africanus and P. uterobilateralis. In Central and South America infection is due to P. mexicanus though the nomenclature is confusing as authors in several countries have published cases as P. peruvianus and P. ecuadorensis among other names. Involved countries include the USA (P. kellicotti), Mexico, Costa Rica, Guatemala, Honduras, Nicaragua, Panama, Colombia, Peru, Venezuela and Brazil. Ecuador apparently has the highest prevalence in the Americas buit surveillance is poor everywhere. Rigorous molecular speciation of Paragonimus sp. in Latin America has not been performed, but there is a suggestion that P. mexicanus, might exhibit some diversity and constitute a species complex <http://www.ncbi.nlm.nih.gov/pubmed/26740357>. Adult flukes live encapsulated in cystic pockets in the lung parenchyma but may also be found in extrapulmonary locations such as skin (case 2007-1). Parasite eggs pass into bronchi and are either coughed up into the environment or swallowed and passed in feces. On reaching fresh water they undergo an obligatory passage through a snail intermediate host and after emerging pass into a crustacean, which is a second intermediate host where they mature to infectious metacercaries which can be transmitted to humans eating undercooked crabs or crayfish. The metacercariae penetrate the duodenum, pass through the diaphragm and travel to the lung parenchyma where they complete maturation. Adult flukes may live for 20 years. Clinically, patients present with cough, sputum, and progressive chest discomfort. The sputum is characteristically tenacious and gelatinous and the hemoptysis generally of a rusty brown color and not bright red. Fever is sometimes present and up to half of patients complain of some dyspnea or wheezing. Eosinophilia is often present. Cysts in the brain are more common in Asia and spinal cord disease may occur. Migratory subcutaneous nodules occur in all species but are most common in P. skrjabini. The patient was treated with praziquantel for 3 days. We would like to thank: Francisco Bravo, Dermatology Faculty |