 |
Gorgas Case 2019-01 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. For the 19th consecutive year, we are pleased to share interesting cases seen by the participants that week during the February/March course offerings. Presently the 9-week Gorgas Course in Clinical Tropical Medicine is in session. New cases will be sent by e-mail every Tuesday/Wednesday for the next 9 weeks. Each case includes a brief history and digital images pertinent to the case. A link to the actual diagnosis and a brief discussion follow.
Carlos Seas and German Henostroza
Course Directors |
|
The following patient was seen in the Tropical Medicine Outpatient Clinic at the Cayetano Heredia Hospital in Lima, Peru during the Gorgas Diploma Course 2019.
 History: A 72-year-old male, previously healthy, presented with a 5-6-year history of right-hand weakness that impaired daily activities. Two years earlier, the patient noticed several, small, circular erythematous lesions on the skin of the abdomen. Lesions were non-pruritic nor painful. During this period, the patient noticed progressive numbness and decreased sensation of the forearms, hands, knees and right foot. He also had an episode of, inadvertently stepping on hot coals and burning his right sole. He denied nasal symptoms as congestion and nosebleeds, and edema of feet.
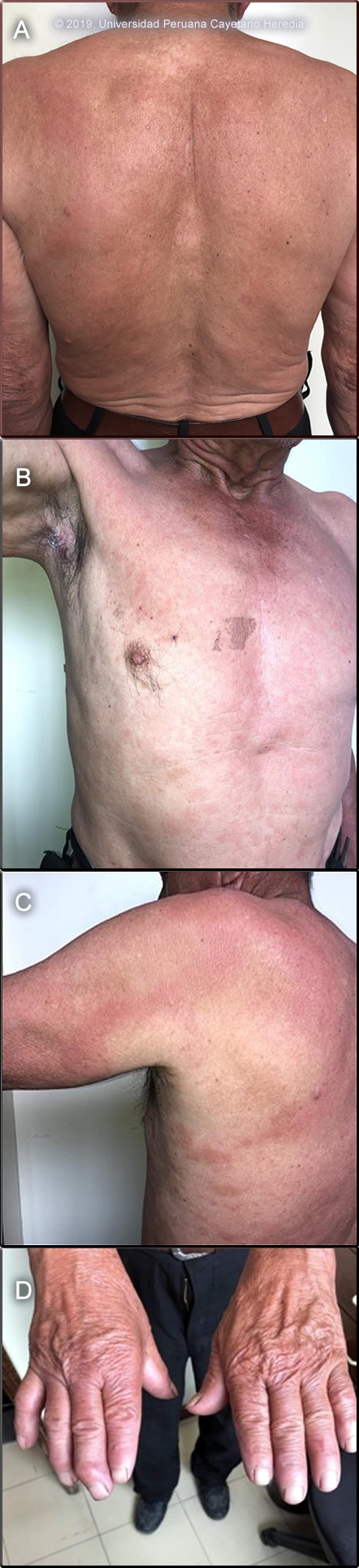
Epidemiology: Lifelong farmer born and lives in Moyobamaba (San Martin, high jungle). No contact with persons with similar lesions. No known TB contacts. No HIV risk factors. Physical Examination: BP: 110/70mmHg. HR: 74. RR 15. Afebrile. No apparent distress. Areas of infiltrated skin with indistinct borders on the upper limbs and trunk [Image A] were seen, as well as multiple small and circular plaques [Image B] extending as far as his thighs and buttocks, and separately a large punched-out plaque was seen over the left scapula and posterior forearm [Image C]. Sensation is impaired in all skin lesions including the center of the large plaque. There is thickening of several peripheral nerves, in particular, the right ulnar and the common peroneal nerves. There is anesthesia in both hands and the right foot, as well as hypoesthesia in the left foot. Additionally, there is weakness in muscles innervated by both ulnar nerves and clawing of the right 5th finger [Image D]. The face appeared normal. Rest of the physical exam is unremarkable. Laboratory: Serological tests for Hepatitis B, C, Syphilis and HIV were negative.
UPCH Case Editors: Carlos Seas, Course Director / Carlos McFarlane, Associate Coordinator UAB Case Editor: David O. Freedman, Course Director Emeritus / German Henostroza, Course Director |
|
Diagnosis: Leprosy (Hansen´s disease) Mycobacterium leprae. Multibacillary leprosy according to the WHO classification. Borderline Lepromatous (BL) leprosy according to the Ridley-Jopling classification.
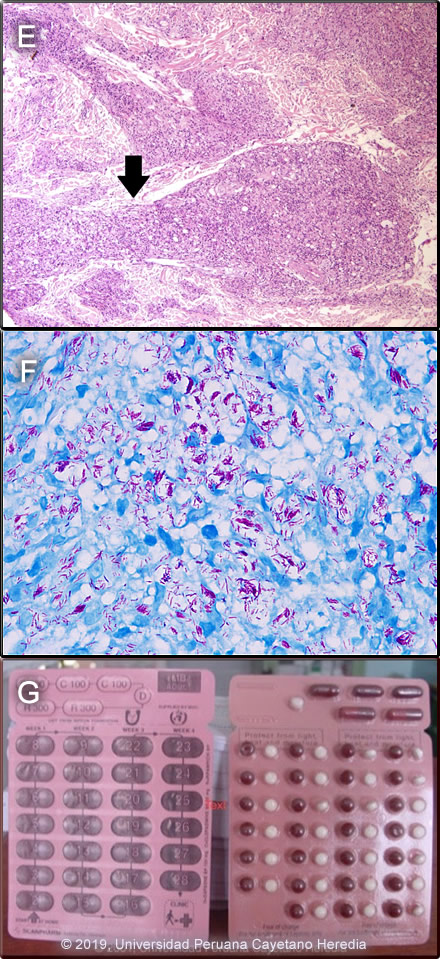
 Discussion: The patient consented to a skin biopsy only from the lesion shown in Image B. Histopathology showed normal epidermis and beneath, in the dermis, there is a dense inflammatory infiltrate, nodular and linear, which is both superficial and deep, and is composed of lymphocytes and foamy histiocytes. The linear infiltrates follow nerve tracts and skin appendix structures [see black arrow in Image E]. The Fite-Faraco AFB stain shows multiple acid-fast bacilli compatible with Mycobacterium leprae [Image F]. These biopsy findings are compatible with borderline lepromatous leprosy when leprosy is classified precisely in the immunologic sense using the traditional Ridley-Jopling classification. This is a spectrum of disease ranging from tuberculoid leprosy (TT) with no AFB in lesions and good cell mediated immunity, to lepromatous leprosy (LL) with many AFB and poor cell-mediated immunity (CMI). In between are the borderline leprosy (BL) patients, borderline tuberculoid (BT) near the tuberculoid end, mid-borderline (BB) in the middle, and borderline lepromatous (BL) near the lepromatous end of the spectrum. The CMI decreases and bacillary load increases as the spectrum goes from TT to LL. Leprosy is a disease of peripheral nerves and skin. Leprosy can be diagnosed clinically in any patient with simultaneous skin lesions and sensory loss over the lesions unless there is hyperkeratosis. However, in early lepromatous cases, sensation is normal over the lesions. Thus, with loss of sensation, a diagnosis of leprosy can be made; with intact sensation, the diagnosis is possible but must be confirmed in some other way. This patient seemed to have three different types of lesions simultaneously: areas of infiltrated skin, multiple small plaques and a large punched-out lesion. Areas of infiltrated skin are characteristic of lepromatous leprosy, areas of innumerable small plaques are characteristic of borderline lepromatous, and the punched-out lesions are characteristic of mid-borderline (BB) leprosy. The polar types of leprosy, TT and LL, are immunologically stable, their CMI never changes, whereas the borderline types are immunologically unstable, their CMI may change over time, they may lose or gain CMI, so their clinical characteristics may change. This patient could have started his illness many years ago somewhere between BT and BL (most skin lesions are compatible with BL), and then decreased his CMI and presented some lesions that resemble early LL, but without other features of LL like nasal symptoms, swelling of feet and facial involvement. For the purposes of determining treatment, the usual and most practical grading system is the WHO classification. For choosing the regimen, it matters only whether the patient has paucibacillary or multibacillary disease. Where no slit skins smears (a test in which a sample of material is collected from a tiny cut in the skin and then stained for M. leprae) can be done, paucibacillary leprosy is defined as five or fewer skin lesions; multibacillary cases have six or more lesions. Paucibacillary disease usually presents with small numbers of hypopigmented macules or erythematous plaques with absent or reduced sensation and well-demarcated borders. Multibacillary disease is usually widespread at diagnosis with multiple plaques or infiltrated areas of skin with indistinct borders that are often non-anesthetic, and papules or nodules. The standard WHO regimen for paucibacillary disease is 100 mg dapsone a day unsupervised and 600 mg rifampin once per month directly observed for 6 months. For multibacillary disease, the long-standing recommendation is for patients to receive 100 mg dapsone and 50 mg clofazimine a day unsupervised and 600 mg rifampin and 300 mg of clofazimine directly observed once per month. A standard WHO multibacillary dose-pack (provided free to endemic countries) is shown [Image G]; the instructions in English must be clarified for all healthcare staff and patients. WHO now recommends only 1 year of therapy for multibacillary cases [controversy discussed in Lancet. 2004 Apr 10;363(9416):1209-19], but some would treat those with high bacterial indices (4 to 6+) for the previously recommended 2 years due to higher relapse rates. For multibacillary disease in the USA and some other developed countries where the cost of rifampin is not limiting, the recommended first line regimen has for many years been 100 mg dapsone, 50 mg clofazimine, and 600 mg rifampin daily for 24 months. No comparative clinical or follow-up data on the different dosing regimens has been published and both are highly effective. However, many patients object to the severe cutaneous pigmentation that results from clofazimine therapy [see Gorgas Case 2005-04] and in the USA minocycline 100 mg/day in place of clofazimine is accepted as an alternative. However, evidence of the efficacy of minocycline’s anti-inflammatory activity against Type 2 reactions (see below) is not as substantial as the evidence for clofazimine. In adults, ofloxacin (400 mg/day) and clarithromycin (500 mg/day) are also sometimes used as a substitute for clofazimine in multi-dose regimens. This patient, being multibacillary, will be treated with the multibacillary regimen recommended by WHO. The possibility of adverse effects of dapsone and clofazimine, or of a lepra reaction should always be explained to a patient who is starting treatment and a reference text should be consulted prior to initiation of therapy by anyone not familiar with these. The most common reaction in multibacillary disease, occurring in about 50% of patients with lepromatous and borderline lepromatous leprosy is a Type 2 reaction, which has as the most common presentation erythema nodosum leprosum (ENL). ENL is a vasculitis at the site of any deposit of dead and disintegrating M. leprae, often accompanied by a severe systemic illness, and characterized by high levels of tissue and circulating TNF-alpha. ENL presents with fever together with many tender erythematous nodules [see Am J Trop Med Hyg. 2006;74(5):868-79]. ENL may also produce to varying degrees, neuritis, uveitis, myositis, dactylitis, periostitis, orchitis, lymphadenitis and nephritis accompanied by edema, arthralgia, and leukocytosis. ENL may occur in patients prior to therapy, during therapy and/or after therapy until the antigen load decreases markedly. ENL may present as repeated acute episodes or may be chronic and ongoing. ENL can be treated symptomatically if mild or with prednisone or thalidomide if severe [see Gorgas Case 2011-04]. In endemic areas, we usually examine the family contacts once a year for at least five years, and advise them to contact the health system in case they present any skin lesion or numbness |