 |
Gorgas Case 2023-02 |
 |
|
The following patient was seen in the Dermatology clinic of Cayetano Heredia Hospital in Lima by the 2023 Gorgas Course participants.
 History: A 32-year-old women presented to the outpatient clinic with a 5-week history starting with a small, erythematous, pruritic papule in the left upper arm which increased in size over the following days. 3 weeks before presentation, she noted purulent and bloody discharge from the lesion, and the lesion became painful when elevating the arm. She sought medical attention, and was prescribed a topical anti-inflammatory and later cephalexin, with no improvement. She presented to our clinic because these symptoms persisted. Epidemiology: Born and lives in Lima. Works as a primary school teacher in the district of Santa Anita. Traveled to Iquitos for tourism 6 weeks prior to presentation, was repeatedly bitten by mosquitoes. No relevant past medical history. Physical Examination: In left upper arm, a 2x2cm pustule with a central punctum, oozing scanty white liquid and bright red blood (Video A). Rest non-contributory.
|
|
Diagnosis: Furuncular myiasis due to Dermatobia hominis. 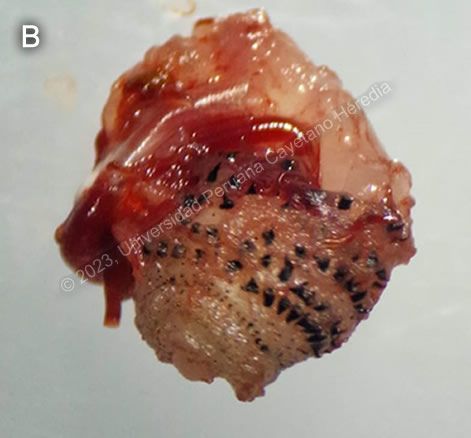
 Discussion: Surgical excision of the larva shown in Image B was performed. Though the typical pear shape of Dermatobia hominia cannot be distinguished, the transverse bands of hooks and respiratory spiracle allow for identification of the species. Myiasis is the infestation of humans and other vertebrates with the larval stages (maggots) of various flies. Flies in several genera may cause myiasis in humans. Dermatobia hominis is the primary human bot fly. Cochliomyia hominivorax is the primary screwworm fly in the New World and Chrysomya bezziana is the Old-World screwworm. Cordylobia anthropophaga is known as the tumbu fly. Flies in the genera Cuterebra, Oestrus and Wohlfahrtia are animal parasites that also occasionally infect humans. D. hominis and C. hominovorax are Neotropical species, ranging from Mexico into South America. Though the epidemiology of furuncular myiasis has not been well described in Peru, cases of D. hominis infestation have been reported in the Northern Coast1 and in travelers in the Amazon basin2,3 and elsewhere4–6. In furuncular myiasis, the larvae penetrate intact living skin but cannot penetrate beyond the subcutaneous tissue, developing into an expanding boil-like lesion. Unlike other fly larvae, D. hominis larvae do not need necrotic tissue, such as an open wound, in order to invade. The adult female fly physically captures a paratenic host, usually a mosquito or tick of a completely different family or arthropods,and then glues her eggs to the abdomen of the carrier mosquito. When the mosquito next feeds on a human or animal, the eggs drop off, hatch and the larva burrows through the skin. Botfly lesions are almost always single, and the furuncle has a characteristic small punctum at the apex through which the larva breathes. Infested persons will usually state that they can feel something moving inside the lesion quite early in the progression of the disease. There are no applicable serological tests, nor are they indicated in the identification of this disease. The diagnosis of myiasis is made by identification of the species of the extracted larva. Treatment consists of removal of the larva, and there is no alternative pharmacological treatment. Occlusion of the respiratory punctum such as with paraffin or petroleum jelly often causes the larva to come out partially on its own and may be curative. If this fails, manual removal is indicated and can be performed by squeezing the larva or by using forceps. However, this procedure can be challenging as the larva has spines on its surface that attach to the host’s tissue. Additionally, the head of the maggot is wider and deeper in the tissue and there is a risk that it could break if pulled. If the maggot is not removed entirely, this could produce severe inflammation. Surgical excision under local anesthesia is necessary for refractory cases; a small cruciate incision around the central punctum facilitates removal of the larva. Bacterial superinfection of Dermatobia hominis furuncles may sometimes occur. Botfly infestation can represent a portal of entry for tetanus, and appropriate prophylaxis should be administered. If not removed, the immature maggot will mature to a pupa over weeks and then drop out and develop into a fly. In Africa, furuncular myiasis is caused by Cordylobia anthropophaga or Tumbu fly (not to be confused with tungiasis caused by the sand flea Tunga penetrans). The Tumbu fly lays eggs on dirty or soiled clothing. If clothing is not properly washed and ironed, the eggs hatch and invade skin when the clothing is next worn. Lesions are almost always numerous and tend to be angrier and more erythematous than with the botfly. Bacterial superinfection is extremely uncommon with Cordylobia anthropophaga. |