 |
Gorgas Case 2023-01 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. For the 23rd consecutive year, we are pleased to share interesting cases seen by the participants that week during the February/March course offerings. Presently the 9-week Gorgas Course in Clinical Tropical Medicine is in session. New cases will be sent by email every Tuesday/Wednesday for the next 9 weeks. Each case includes a brief history and digital images pertinent to the case. A link to the diagnosis and a brief discussion follows. Carlos Seas and German Henostroza |
|
The following patient was seen in the Pulmonology Ward at the Cayetano Heredia Hospital in Lima, Peru during the Gorgas Diploma Course 2023.
 History: A 54-year-old woman presents with a 1-year history of dyspnea on exertion associated with interscapular pain which worsen over time and start affecting her daily activities; she seeks medical attention through our emergency department. No history of fever, vomiting or weight loss. No other significant past medical history. Epidemiology: Born in Cajatambo, in the highlands of Lima region, and lives in Jucal, also in the highlands of Lima. Used to work on a farm with sheep, pigs and horses, now works as a homemaker. Physical Examination: BP 90/60 mmHg, HR 65 bpm, RR 21 rpm, SatO2 92% on room air. Decreased air entry in right hemithorax and rales in left hemithorax. Rest unremarkable. Laboratory: Hemoglobin 13, hematocrit 39. Leucocytes 4.32 (0% bands, 57% segmented, 3.6% eosinophils, 0.6% basophils, 7.5% monocytes, 31% lymphocytes). Platelets 293 000. INR 0.93, PT 12.8, aPTT 31.3.
|
|
Diagnosis: Echinococcus granulosus. Complicated cyst in left hemithorax and intact cyst in right hemithorax. 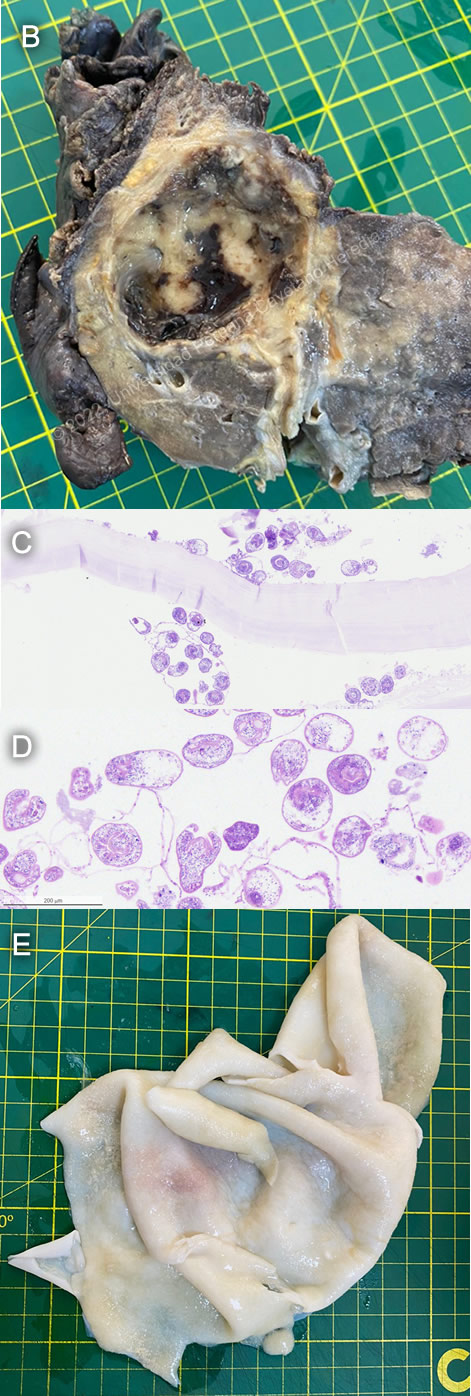
 Discussion: A diagnosis of cystic echinococcosis with a complicated cyst in the left hemithorax and intact cyst in right hemithorax was made on the basis of CT imaging, which was lost during the hospitalization. The patient first underwent a cystectomy and capitonnage to remove the left complicated cyst, which was filled with purulent, foul-smelling material that connected with the bronchial tree but not with the pleura (Image B). It is important to note that not all patients will report a history of “hydatid vomica", a term that refers to expectoration of transparent, salty cyst contents through the mouth and nose, even if cysts break into the bronchial tree. Results from a chest CT would have been useful to assess the patient prior to surgery and determine if there was rupture of the cyst into the thoracic cavity, which would have drastically changed the prognosis. Unfortunately, tomography is not always readily available in our setting. In addition to a cystectomy, a bronchial lavage was performed, and microscopic examination of the samples obtained during this procedure revealed the classic histology of a thick acellular laminated membrane with multiple protoscolices of E. granulosus (Image C and D). After recovery, the patient underwent a right superior lobectomy to remove the uncomplicated cyst (Image E), which occupied 90% of the right superior lobe. Hydatidosis is caused by the larval form of Echinococcus granulosus, the dog tapeworm. Humans become accidental intermediate hosts after ingesting tapeworm eggs in dog feces. Larvae grow in cysts in the liver and/or lungs and expand slowly over the year, usually with no symptoms until they grow to large sizes and start impinging on important structures, or if they rupture or become infected. In the case of the presented patient, symptoms likely began when the cyst in the left hemithorax ruptured. Management of hydatid disease depends on the location and size of the cysts. Small, simple cysts (<5 cm in diameter) may be treated only with antiparasitic therapy with albendazole. Percutaneous treatment via puncture, aspiration, injection and reaspiration (PAIR) is a less invasive alternative to surgery but is only done for liver cysts without daughter cysts, so was not an option for our patient. Surgery is the treatment of choice for extrahepatic cysts, complicated cysts and cysts larger than 10cm in diameter. It is important to avoid spilling the contents of the cysts, as this may seed protoscolices in the cavity leading to further disease or cause anaphylaxis. The timing of adjunctive antiparasitic treatment for cases requiring surgery is a cause of controversy: some literature suggests that preoperative albendazole minimizes the risk of secondary seeding via a decrease in viability of the cyst (https://pubmed.ncbi.nlm.nih.gov/18819855/); however, there is anecdotal evidence at our institution suggesting that preoperative antiparasitics may weaken the wall of the cyst and increase risk of rupture. Thus, our patient did not receive albendazole until after her surgeries. She continues to be closely monitored for complications. |