 |
Gorgas Case 2025-1 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. For the 29th consecutive year, we are pleased to share interesting cases seen by the participants that week during the February/March course offerings. Presently, the 9-week Gorgas Course in Clinical Tropical Medicine is in session. New cases will be emailed every Tuesday/Wednesday for 9 weeks. Each case includes a brief history and digital images pertinent to the case. A diagnosis and a short discussion follows.
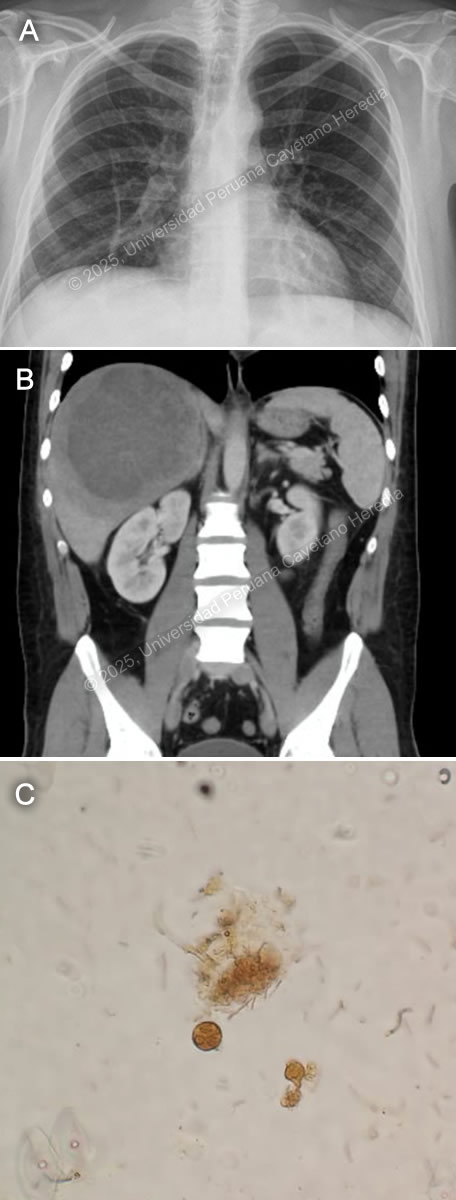 History: A 34-year-old male patient with no significant PMH presented to the ED with a 2-week history of abdominal pain and subjective fevers. Two weeks before admission, he presented epigastric pain associated with nausea, decreased appetite, and fever quantified at 39 C. One week before admission, right pleuritic chest pain was added. Symptoms persisted, and on the day of admission, an abdominal US revealed hepatomegaly with a 13.4 x 3.6cm heterogeneous liver lesion. Epidemiology: The patient was born in Lima, Peru's capital, but currently lives in the city of Tumbes, in the northern part of the country’s coastline. He works as an independent vendor in the textile industry and constantly travels from Lima to Tumbes. While in Tumbes, he endorses eating raw vegetables, abundant seafood, including blood clam ceviche, from street vendors and drinking non-potable water. Two weeks before the onset of symptoms, he reported two weeks of self-limited watery diarrhea. Physical Examination on admission: BP: 120/80 mmHg; RR: 18; HR: 88; T: 38.4 °C, Sp02 97% on room air. The patient didn't appear to be in any acute distress. There was no skin rash or jaundice and no palpable lymphadenopathy. His abdomen was mildly distended, with epigastric tenderness on palpation. Hepatomegaly with point tenderness 3cm below the right costal margin was found. The rest of the exam was normal. Laboratory: Hemoglobin was 14.4 g/dL, WBC 26 000/uL with no bands, 22100/uL neutrophils, 1300/uL lymphocytes, no eosinophils, no basophils, and 1820/uL monocytes. Platelets were 429 000/uL. PT was 15 sec, PTT 30 sec with an INR 1.26. Total bilirubin was 2.9 g/dL with a direct bilirubin of 1.8 g/dL. Alkaline phosphatase was 307 UI/L (20-140 UI/L) with an albumin of 2.8 g/dL (3-4 g/dL). Sodium was 134 mEq/L (135-145 mEq/L), potassium 4.4 mEq/L (3.5-5.5 mEq/L), and chloride was 94 mEq/L (96-106 mEq/L). Imaging: A chest X-ray was performed, revealing elevation of the right hemidiaphragm (Image A). An abdominal CT scan without contrast revealed an approximately 12-15cm in diameter hypodense lesion with well-demarcated borders in the right hepatic lobe (Image B). Stool ova and parasite was performed (Image C). UPCH Case Editors: Carlos Seas, Course Director / Mario Suito, Associate Coordinator |
|
  Discussion: US-guided percutaneous catheter drainage (PCD) of the liver lesion was performed (Video), revealing an anchovy paste-appearing fluid (Image D). Abscess direct microscopy for ova and parasites (O&P) was negative. Galactose/ Galactose- N-acetylcysteine (Gal/GalNAC) lectin antigen from the abscess was positive, as well as total serum anti-Gal/GalNAC antibodies for Entamoeba histolytica antibodies, confirming the diagnosis. Image C shows a cyst of E. histolytica in the stools, featuring a rounded structure with three nuclei (lugol stain). An amebic liver abscess (ALA) is the most common extra intestinal complication of Entamoeba histolytica infection. The disease remains prevalent in developing nations, particularly in rural areas with poor sanitation in India, South America, and Africa (1). ALA is 10 times more common in men between 30-50 years than in women and it tends to be more severe in older patients (2, 3). Alcohol consumption is a major risk factor (4), and the right lobe of the liver is involved in 80% of cases, usually solitary with variable size (5). ALA is the most common cause of liver abscesses in the developing world. This disease is caused by E. histolytica trophozoites that invade the liver through the portal circulation after ingestion of contaminated food or water by E. histolytica cysts, which hatch in the small intestine and penetrate the colonic mucosa, where they cause amebic colitis (5). Unlike pyogenic liver abscesses, ALA is non-suppurative and consists of necrotic hepatocytes and cellular debris caused by the phagocytic ingestion of cells in bites, also known as ‘’trogocytosis-like’’ (6). ALA is classified into three clinical forms: subacute mild, acute aggressive and chronic indolent. The most common (80%) is the subacute mild form, with moderate symptoms and good response to medical therapy. Acute aggressive ALA usually presents with a rapidly progressive course and high risk of rupture. Chronic indolent ALA shows prolonged symptoms, thick fibrotic walls, and potential for secondary bacterial infection (5). The classic clinical presentation includes fever, right upper quadrant pain, and hepatomegaly. Jaundice and pleuropulmonary symptoms occur in a minority of cases (7). Complications arise from rupture, secondary infections, or vascular events. Rupture occurs in 6–40% of cases and can lead to peritonitis, pleural empyema, hepatobronchial fistula, or pericardial tamponade (5, 8). Vascular complications include thrombosis of the hepatic and portal veins, leading to ischemia, portal hypertension, and Budd-Chiari syndrome (6). The differential diagnosis of the liver lesion includes pyogenic liver abscess, cystic echinococcosis, hypervirulent Klebsiella pneumoniae infection, and primary liver malignancy. Diagnosis is based on clinical presentation, imaging such as ultrasound or CT scan, and serological, antigenic, or molecular tests. Serology is of limited use in endemic countries due to the high seroprevalence (1, 8). Abscess drainage confirms the diagnosis by finding the classic “anchovy paste” aspirate and, more specifically, Gal/GalNAC lectin antigen detection. A possible alternative to diagnostic drainage is serum antigen detection, which is highly sensitive but not routinely available. Stool O&P is neither sensitive nor specific (5). The first-line treatment for ALA is metronidazole 500–750 mg TID for 7–10 days, followed by a luminal amebicide to prevent recurrence (6). Most uncomplicated cases respond to antibiotics alone. However, percutaneous drainage (PCD) is required for: 1) large abscesses (>5–10 cm), 2) non-resolving symptoms after 72–96 hours, 3) high-risk locations (left lobe, subcapsular, caudate lobe), 4) secondary infection or rupture. Surgical drainage is reserved for cases with extensive peritonitis or failure of PCD (1, 6). Our patient had a big abscess that merited drainage. He is receiving metronidazole with complete resolution of symptoms; fever disappeared after 2 days of antibiotic treatment. References |