 |
Gorgas Case 2025-11 |
 |
|
This is the last case of the week of 2025. The cases have been selected and edited by the Directors and Clinical Coordinator of the Courses. We want to express our gratitude to everyone involved in preparing these cases. We will post new cases in 2026.
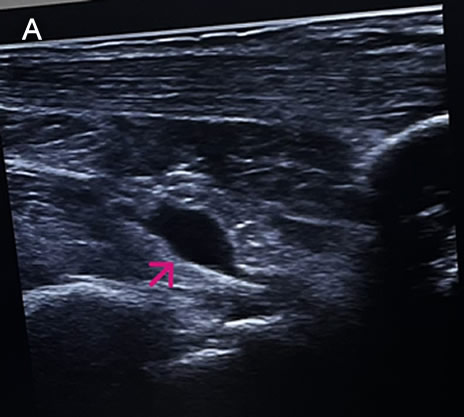 History: A 73-year-old female patient with a past medical history of arterial hypertension presented with a 2-month history of polyarthralgias and subjective fever. Two months before admission, while in Santa Cruz, Bolivia, the patient began experiencing a subjective fever accompanied by chills. One day following symptom onset, she developed severe joint pain involving both wrists, shoulders, and ankles. Two days later, she reported decreased appetite, nausea, vomiting (4–5 episodes per day), and watery diarrhea (6–7 episodes per day). On day 3 of illness, the patient developed localized swelling over the dorsum of the right foot. She received symptomatic treatment with minimal pain relief. One month before admission, the patient experienced severe upper limb pain, which impaired her ability to raise her arms or hold objects, along with intense ankle pain that significantly limited walking. She was evaluated at the rheumatology service and subsequently referred to our outpatient clinic. Epidemiology: The patient was born and currently resides in Lima. She currently has no occupation. She traveled to Santa Cruz, Bolivia, from March to June of the present year to visit her son. There, she reports visiting many tourist attractions, including areas of the highlands and the jungle, where she sustained numerous mosquito bites. Physical Examination on admission: BP: 130/80, RR: 18, HR 87, SpO2: 97% on room air. Musculoskeletal examination revealed tenderness on palpation of the metacarpophalangeal joints, decreased grip strength, and pain with passive and active movement of both shoulders. Additionally, tenderness was noted on palpation of the popliteal region, both knees, and both ankles. The patient presented with difficulty walking due to persistent pain. The rest of the exam was non-contributory. Laboratory: Hemoglobin 12.9g/dL, Hematocrit 36.2%, Platelets 222000, WBC 4500, /µL; with bands 1%, neutrophils 49%, eosinophils 5%, basophils 0%, monocytes 0%, lymphocytes 45% Glucose 88 mg/dl, Urea 42 mg/dl, total proteins 7.15 g/l, albumin 4.07 g/l. The urine exam was normal. An Ultrasound examination demonstrates bilateral synovitis involving the wrist joints and popliteal regions, characterized by joint effusion and synovial thickening. Additionally, there is evidence of bilateral tenosynovitis of the Achilles tendons, characterized by hypoechoic peritendinous fluid and thickening of the synovial sheath. Evaluation of the hindfoot reveals retrocalcaneal bursitis, manifested by distention of the retrocalcaneal bursae with anechoic fluid (IMAGE A, see arrow). UPCH Case Editors: Carlos Seas, Course Director / Paola Nakazaki, Associate Coordinator |
|
Discussion: The skin scrape microscopy shows structures typical of Sarcoptes scabiei. An ELISA test for detecting IgM antibodies against the Chikungunya virus was positive. Chikungunya virus is an arthropod-borne alphavirus in the Togaviridae family, transmitted by mosquitoes, mainly Aedes aegypti and Aedes albopictus. It was first identified in East Africa during the 1950s. It was called kungunyala, meaning “to walk bent over” or “to become contorted,” due to the severe pain often associated with the illness (1). Chikungunya is now widespread across tropical and subtropical regions of Africa, Asia, the Americas, and, to a lesser extent, Europe, primarily through travel-related cases (2). The incubation period typically ranges from 2 to 6 days. Less than 15% of infected individuals remain asymptomatic. At the same time, most individuals develop symptoms, typically starting with fever and malaise, which can be accompanied by musculoskeletal manifestations that may even precede fever, such as arthralgias and myalgias, or dermatologic involvement. In most cases, this includes an erythematous maculopapular rash that primarily affects the trunk but can also extend to the face and extremities (3). Arthralgias are usually bilateral and more often affect distal joints, with hands, wrists, and ankles being the most commonly involved areas. They may also be accompanied by tenosynovitis or periarticular swelling. The acute phase typically lasts between 1 and 2 weeks, characterized by a high-grade fever that typically lasts for three to five days. Musculoskeletal symptoms may persist chronically in around 30% of cases (4,5). Less common manifestations include lymphadenopathy, pruritus, and gastrointestinal symptoms, which can appear after viremia has resolved (3). Chikungunya infection should be clinically suspected in patients with epidemiologic exposure, considering the differential diagnosis of other conditions such as dengue fever, oropouche, Zika virus, leptospirosis, malaria, and rheumatoid or reactive arthritis. The diagnosis is established by PCR detection of chikungunya viral RNA, especially in those who present within the first week of symptom onset, or by serology in patients with symptoms lasting more than one week. ELISA can detect IgM within five days of symptom onset and can persist for weeks to months (3,6). There is no specific antiviral treatment for chikungunya virus infection. Management is supportive and symptomatic. The main aspects of therapy include rest, proper hydration, and relief of fever and joint pain with acetaminophen. NSAIDs can be used for persistent arthralgia after confirming dengue has been ruled out. For patients who develop chronic arthritis or arthralgias, corticosteroids and certain antirheumatic drugs, such as methotrexate, have been effective in small, randomized trials and observational studies (7,8). Currently, there are two approved vaccines: a live-attenuated vaccine (IXCHIQ) indicated for adults 18 and older, and a virus-like particle vaccine (Vimkunya) for individuals 12 and older. Protection against infection is 40%, and against disease is 70%. The vaccines are mainly recommended for travelers and laboratory workers; they are also used in areas where outbreaks have been identified. The IXCHIQ has caused serious adverse events in people 60 and older. The FDA, CDC, and EMA have ceased their indication for that age group, and the WHO has taken a cautious stance. Our patient sought care at our Institute after 2 months of symptom onset due to persistent pain that caused difficulty walking (VIDEO A), decreased grip strength (VIDEO B), and impacted her ability to perform daily activities. She is part of the subset of patients who continue to have chronic musculoskeletal involvement. She received symptomatic treatment with orphenadrine and celecoxib, and a drainage procedure was performed on the fluid in the retrocalcaneal bursae, as previously described in the ultrasound, with reported pain improvement at the follow-up visit. References |