 |
Gorgas Case 2025-5 |
 |
|
The following patient was seen in Cuzco by the 2025 Gorgas Course participants.
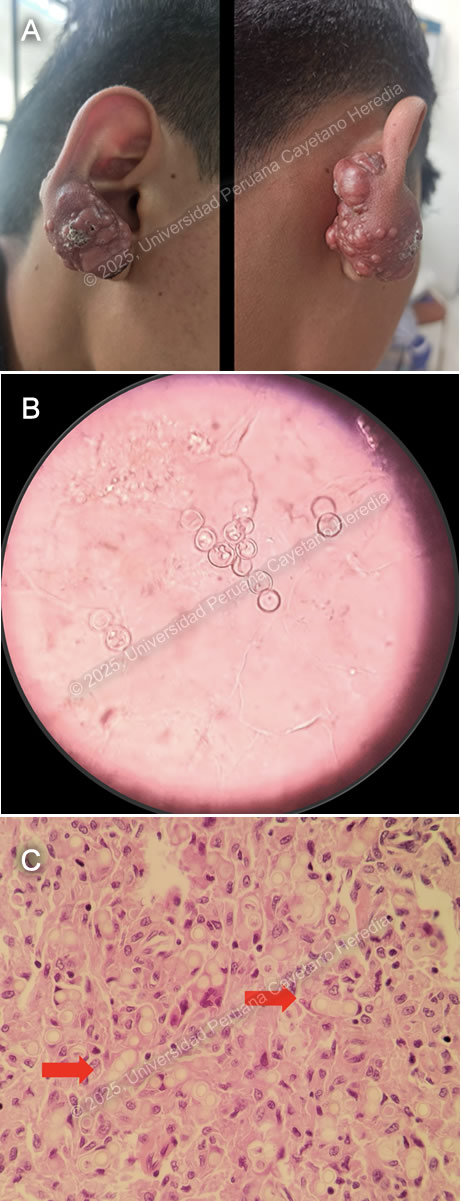 History: A 17-year-old male patient with a history of epilepsy presented to the outpatient clinic in Cuzco with a 10-year history of a progressive lesion on his right earlobe. Ten years before admission, he noticed a non-painful, non-pruritic, papule-like lesion on his right earlobe. The lesion increased significantly in size, prompting surgical removal seven years before admission. Unfortunately, the lesion recurred after surgery with a faster growth rate, developing a tumor-like, verrucous appearance, associated with burning pain and pruritus.. The lesion was non-anesthetic, had no drainage or fistulation, and was not associated with systemic symptoms or evidence of metastatic disease. Epidemiology: The patient was born and raised in Cuzco, a highland city in Peru. Fourteen years before admission, he traveled with his father to Madre de Dios in the low jungle of Peru, where he stayed for two years. He returned to Madre de Dios for two weeks one year before admission. He also reported contact with a cousin who had tuberculous meningitis. Physical Examination on admission: BP 100/60 mmHg, RR 18 breaths per minute, HR 71 bpm, Temp 36.4°C, SpO₂ 92% on room air. A tumor-like exophytic lesion with multiple nodules and superficial crusting was noted on the helix and lobule of the right earlobe (Image A). The lesion was firm and hard to touch, with no discharge, regional lymphadenopathy, or sinus tracts. The rest of the physical exam was within normal limits. Laboratory: Hb: 18.7 g/dL (Hematocrit: 54%); Leukocytes: 10,260/µL (Neutrophils: 7,120/µL, Eosinophils: 120/µL, Lymphocytes: 2,370/µL); Platelets: 397,000/µL; Glucose: 97 mg/dL; Urea/Creatinine: 30/1.16 mg/dL; AST/ALT: 27/37 U/L; Alkaline Phosphatase: 119 U/L; Albumin: 4.5 g/dL; Sputum AFB x2: Negative. HIV, HTLV-1, Syphilis, HBsAg, Anti-HBc, and HCV non-reactive. UPCH Case Editors: Carlos Seas, Course Director / Mario Suito, Associate Coordinator |
|
Discussion: Both KOH-stained light microscopy and histopathology revealed fungal structures compatible with Paracoccidioides loboi. Lobomycosis is an exceedingly rare subcutaneous mycosis caused by the yet unculturable and recently renamed Paracoccidioides loboi (formerly Lacazia loboi). Accidental trauma, particularly involving plants and thorns, is thought to be the primary transmission mode, although not in all cases (1). The latest prevalence estimates report 907 total cases of lobomycosis, with 55% of cases originating in Acre State, Brazil (2). The remaining cases come from the Amazonian rainforest regions of Brazil, Peru, and Colombia. Cases in developed countries such as the United States have been reported in migrants or tourists returning from endemic areas (3). Notably, bottlenose dolphins have also been found to be affected by this disease. Lobomycosis remains restricted to the skin and typically follows a decades-long progression. The classical lesions are red, hard, shiny keloidal plaques or nodules that may ulcerate with secondary crusting or develop a verrucous appearance over time. Local extension is the norm, and there have been no reported cases of metastatic disease. The most common sites of involvement are the lower extremities, followed by the ears, upper extremities, and head. Disseminated cases have been described, presenting with multifocal lesions, intense pruritus, and marked ulceration. The diagnosis is confirmed by direct visualization of fungal cells in KOH-stained light microscopy or histopathological analysis of clinical specimens, revealing round 9-µm single or short-chain yeast cells with thick double cell walls. Specimens for light microscopy can be obtained using the “Scotch tape test,” where vinyl adhesive tape is applied to the crusted lesion and transferred to a glass slide for KOH staining. Histopathology (Hematoxylin-eosin or Grocott-Gomori staining) is the gold standard diagnostic test (3). Since P. loboi has not been successfully cultured, 18S ribosomal analysis has revealed its close relation to Paracoccidioides brasiliensis (4) The main differential diagnosis includes bacterial infections such as cutaneous TB (Tuberculosis verrucosa cutis), non-tuberculous mycobacteria (NTM) infections, actinomycetoma, and botryomycosis; fungal infections such as paracoccidioidomycosis, eumycetoma, sporotrichosis, and chromoblastomycosis; and parasitic infections such as cutaneous leishmaniasis (5) There is no curative treatment for lobomycosis. Surgery is an option, though primarily for cosmetic purposes. Case reports have described successful treatment with posaconazole, clofazimine, and itraconazole (6-8). Our patient was treated with 1 month of TMP/SMX and itraconazole, but no significant clinical response was observed, leading to surgical removal of the lesion. References |