Optimizing Obstetric Care Quality Initiative
The Optimizing Obstetric Care Quality Initiative was launched to address persistently elevated obstetric length of stay (LOS), which had drifted two standard deviations above peer benchmarks. Early review demonstrated a multifactorial problem rooted in inconsistent discharge expectations, gaps in hypertension management, unaddressed social needs, and communication challenges across teams. Given the breadth of contributors, the project engaged a wide interdisciplinary stakeholder group, including physicians and nurses across the obstetric continuum (MEU, L&D, HROB, MBU, NBN, RNICU, CCN), as well as Social Work, Care Integration, HSIS, and Community Health Equity services.
Using structured quality improvement methodology, the team identified barriers, defined the current process, collected baseline data, and prioritized targeted interventions. Several high-impact changes were implemented throughout 2024. Hypertension management guidelines launched in April, standardizing care for a key contributor to prolonged stays. In November, a new Milestone Checklist was introduced to improve consistency of discharge expectations and align teams around key readiness indicators. Additional improvements included enhanced inpatient–outpatient social work communication (implemented in October) and updated Rose’s Law scripting to strengthen family-centered communication across all units.
These interventions have generated meaningful improvements. Cesarean section LOS decreased from 5.95 to 4.96 days, and patients with hypertension who underwent a cesarean section had a LOS that decreased from 6.71 to 5.53 days. Leadership rounding has provided anecdotal confirmation of more patients being discharged within the recommended 48–72-hour timeframe. Adoption of the Milestone Checklist has been consistent, reinforcing a more predictable and coordinated discharge process.
Success has been driven in large part by exceptional leadership engagement, with leaders across units taking clear ownership of the project and promoting cultural alignment around LOS improvement. Challenges remain around the precision of available data—specifically, developing reliable measures of intervention compliance and addressing nuances in data capture that affect LOS reporting—but these issues are being actively addressed.
The project is now in the sustainment phase. The MBU/NBN Accountable Care Team has incorporated ongoing LOS review into its standing workflow. A comprehensive resource and referral list addressing patients’ social needs has been collated with ongoing maintenance needs. Work continues to refine inaccurate postpartum MS-DRG capture from a clinical perspective within the coding guidelines, which currently inflates LOS values in Vizient. Additional efforts are focused on improving follow-up appointment adherence to reduce readmissions.
Overall, this initiative demonstrates strong multidisciplinary collaboration, measurable improvements in outcomes, and a clear roadmap for continued progress. It represents a successful model for sustained quality improvement within the obstetric service line.
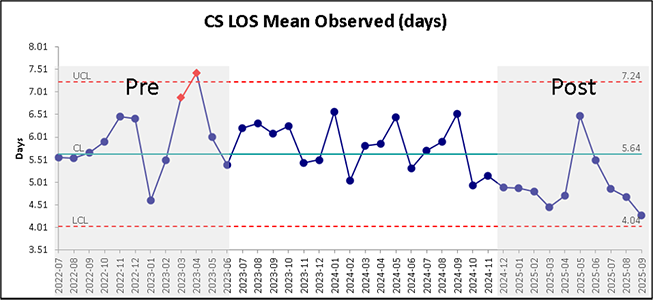
Figure 1. Cesarean Section LOS
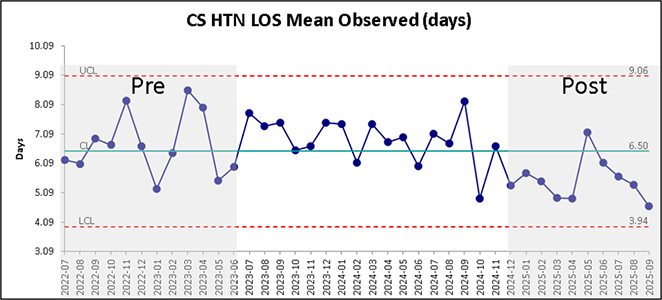
Figure 2. Cesarean Section Complicated by Hypertension LOS
Anemia in Pregnancy Quality Improvement Initiative
The goal of this project is to implement a new screening and management plan for all obstetric patients aimed at reducing pre-delivery anemia (hemoglobin <10.6 mg/dL). The new protocol, which was implemented in October 2023, includes adding a ferritin level to routine labs (complete blood count and hemoglobin electrophoresis) to assess for iron deficiency. This ideally allows for earlier detection of iron deficiency and prevention/treatment of iron deficiency anemia.
In the first 6 months of the protocol, we have seen outstanding results. Pre-delivery anemia has decreased from 29% pre-intervention to 19% post-intervention (p<0.001) with a similar reduction in moderate/severe anemia (hemoglobin <9.0 mg/dL). The monthly mean of patients with pre-delivery anemia is demonstrated in Figure 1. Since the protocol was implemented, the rate of patients having a ferritin drawn during pregnancy has increased from 9% to 80.5%, demonstrating an effective compliance rate. Rate of infusion reactions have been tracked for safety monitoring, and while the reported infusion reaction rate between January to June 2024 was 10%, all of these reactions were either classified as mild (“fishbane reaction”, 57%) or as an isolated symptom (43%). There were no cases of anaphylaxis. Infusion reaction monitoring remains ongoing.
Overall, these results are promising. Future steps for the initiative include tracking rates of blood transfusions to determine if reducing pre-delivery anemia has an effective on the need for peridelivery transfusion.
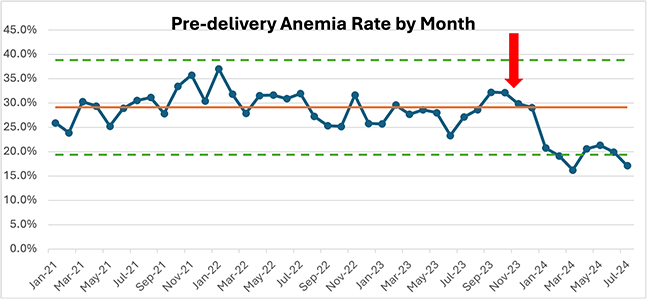
Figure 1. Pre-delivery anemia rate by month. The solid orange line represents the mean number of patients with pre-delivery anemia (hemoglobin <10.6 mg/dL) during the pre-intervention period (January 2021 to September 2023). The green dashed lines represent the upper and lower control limits which are +/- 3 standard deviations from the historical mean. The blue line indicates the monthly mean for pre-delivery anemia. The red arrow indicates the start of the new protocol. Since January 2024, the rate of anemia has been lower than the historical mean indicated a statistically significant decrease in pre-delivery anemia (p<0.001).
Restriction Opioid Prescribing Algorithm
Over the past two decades, opioid-related deaths have increased in the United States by six times and the Department of Health and Human Services has declared the opioid crisis a public health emergency. The overuse of prescription opioids has contributed to the subsequent epidemics of misuse, abuse, and increased morbidity and mortality. Prescription opioids are utilized across all surgical subspecialties and are the mainstay for postoperative pain management in gynecologic oncology patients. Traditionally, patients have been overprescribed opioids postoperatively, leading to chronic use in 5-10% of gynecologic patients. Currently, most surgeons have wide variance in the number of pills prescribed for common procedures and generally overprescribe for patients undergoing surgery with up to 70% of pills not taken by the patient.
Increased awareness of opioid prescribing practices is being accomplished by implementation of multimodal pain control through enhanced recovery programs (ERPs) and developing opioid stewardship guidelines, all while setting patients' expectations and managing their pain. There is evidence to show that a restrictive approach is effective in reducing the number of opioids prescribed to patients after undergoing gynecologic surgery. The objective of this study was to evaluate the impact of and patient satisfaction with a restrictive opioid prescribing algorithm (ROPA) in gynecologic oncology patients undergoing surgery
We implemented this program in August 2018 for gynecologic oncology patients undergoing any surgical procedure. Patients were educated preoperatively about pain management goals, restrictive opioid use, and opioid disposal. A 4-tiered system was developed to standardize prescriptions at discharge based on surgical complexity and inpatient opioid requirements. Patients were surveyed at their postoperative visit to assess home opioid use and satisfaction.
After the first year of the program, patients were compared to historical controls managed without a ROPA from 10/2016-9/2017. 2,549 patients were included in the study. 1,321 patients in the control group and 1,228 patients in the ROPA group. Compared with the control group, the average number of opioid pills prescribed was significantly lower in the ROPA group (30.5 vs 11.3). The percentage of patients requiring opioid refill within 30 days was similar (13.0% vs. 12.6%). 95.7% of patients surveyed were satisfied with their pain regimen. The total number of pills prescribed annually decreased from 34,130 in the control group to 13,888 in the ROPA group. The numbers of pill prescribed in 2020 continued to decrease (11,207).
A restrictive prescribing practice allows for a significantly lower number of opioids to be prescribed to postoperative patients while maintaining patient satisfaction. There was no increase in opioid refill requests using a restrictive algorithm in patients undergoing gynecologic surgery.
Obstetrics Hemorrhage Protocol
Postpartum hemorrhage (PPH) is a leading cause of maternal mortality and complicates between 1-5% of deliveries. The unpredictable nature of postpartum hemorrhage has prompted development of protocols for early detection and management. Due to the subjective and inaccurate nature of visual estimated blood loss, the National Partnership for Maternal Safety encourages formal efforts to quantitate blood loss at delivery.
We utilized data captured during a pilot evaluation of colorimetric technology and gravimetric techniques assessing quantitative blood loss at delivery to establish “blood loss cutoffs” for vaginal and cesarean deliveries. These cutoffs include number of sponges utilized during delivery and captured blood in suction canisters or graduated vaginal delivery drapes.
According to our data, 7% of women who delivered spontaneously had greater than five sponges used during delivery and 90% of these women had less than 500 cc in the graduated delivery drape. Based on this, we established the “5/500 rule” for vaginal deliveries. Similarly, 10% of women delivered by cesarean had greater than 30 laparotomy sponges used during surgery and 92% had less than 300 cc of blood in the suction canister after surgery. Based on this we established the “30/300 rule” for cesarean deliveries.
If any of these sponge count or volume thresholds are met, regardless of provider estimated blood loss, an Obstetrics Hemorrhage Protocol is activated through a PowerPlan that includes increased blood pressure and urine output surveillance on L&D with serial hemoglobin values for a period of 4 – 6 hours. This increased surveillance identifies those patients who may benefit from earlier intervention, including transfusion, to avoid the maternal consequences of unrecognized blood loss at delivery. This protocol allows patients to remain in L&D for observation and recognition of ongoing bleeding or decompensation.
OASIS Protocol
Obstetric anal sphincter injuries (OASIS) occur in approximately 6-7% of vaginal deliveries and may result in loss of bowel control, increase risk of injury in subsequent deliveries, and negatively affect quality of life. It is important for women at risk (vaginal delivery, operative vaginal delivery, episiotomy, increased fetal birth weight, and induction of labor) to be identified. For those women who sustain an injury, it is vital that they are accurately diagnosed and managed in a standardized, evidence-based manner to minimize morbidity and optimize recovery.
The aim of this project was to evaluate the literature with regard to intrapartum prevention, postpartum repair, and post-discharge management of OASIS. Subsequently, we created an OASIS quality care bundle which included prospective follow-up in a Postpartum Perineal Clinic to collect outcomes of women undergoing childbirth at a quaternary care center. A secondary aim is to evaluate the incidence and describe outcomes of women who sustain an injury before and after the OASIS quality care bundle was implemented. A protocol for management of OASIS was created with input from experienced clinicians. Patients who sustained a 3rd or 4th degree perineal laceration during childbirth from January 2017 to September 2019 comprised the pre-QI care plan population. Baseline demographics as well as intrapartum and postpartum variables were collected.
In October 2019, we introduced an evidence-based educational program in the form of didactic instruction regarding optimal intrapartum care, recognition, diagnosis, surgical repair, and postpartum care of OASIS. Experienced providers taught surgical repair simulation sessions. A standardized OASIS quality care bundle was implemented. Patients were evaluated in a Postpartum Perineal Clinic by urogynecologists 2 weeks, 6 weeks and 6 months postpartum. At these visits, patients completed validated questionnaires. The post-QI care plan population consisted of women sustaining OASIS from October 2019 through July 2021. Demographic, intrapartum, and postpartum outcome data were prospectively collected to compare pre-QI care plan outcomes to post-QI care plan outcomes.
Prior to care bundle implementation, 98 cases of OASIS were identified. 87% of these were 3rd degree lacerations. 73% of women who sustained an OASIS were nulliparous and 39% of OASIS resulted from operative vaginal delivery. Those who underwent operative vaginal delivery spent on average twice as long in the second stage of labor than those that delivered spontaneously (135 vs 77 minutes, p<0.001) and had higher birthweight (3530g vs 3285g, p=0.02). Post care bundle implementation, 80 women with OASIS were identified. 83% of these were 3rd degree lacerations. 33% of the total OASIS resulted from operative vaginal delivery. Pre- and post-QI groups did not differ with regard to age or race. Additional demographics and outcome variables are being collected and analyzed.
Implementation of an evidence-based OASIS quality care bundle plan for management of women sustaining an OASIS at the time of vaginal delivery resulted in increased awareness of optimal care of women sustaining OASIS and has allowed for standardization of care as well as tracking of outcomes. Analyses are in process and will be used to determine whether the quality care bundle affected outcomes in women sustaining OASIS.