
For a fungus, there is no place like Alabama.
“Alabama is a hotbed for fungal diseases,” said Peter G. Pappas, M.D., professor in the Division of Infectious Diseases in the UAB Heersink School of Medicine. “We see as much or more in the way of fungal infections as anyone in the country.” Pappas is a leader of the Mycoses Study Group, a world-renowned, UAB-administered group of experts who focus on understanding and treating invasive fungal infections and have led most of the clinical trials for FDA-approved antifungal treatments. (Mycology is the study of fungi; mycoses are invasive fungal infections.)
Why do fungi love Alabama? Geography is one big reason. “We are in the hot, humid Deep South, and our soil and flora contribute as well,” Pappas said. This is not necessarily a bad thing. “If fungi weren’t here, the Earth would be covered with plants and trees and organisms that had never decayed,” Pappas said. “Their primary purpose is to break down organic material into its elementary components. Sadly, they can do the same thing to people.” And unfortunately, “our population in Alabama tends to be sicker” and immunocompromised, Pappas said. “We have a large group of transplant recipients, HIV patients and people on immunomodulation therapy for diseases such as lupus. The environment in Alabama is like the perfect storm.”
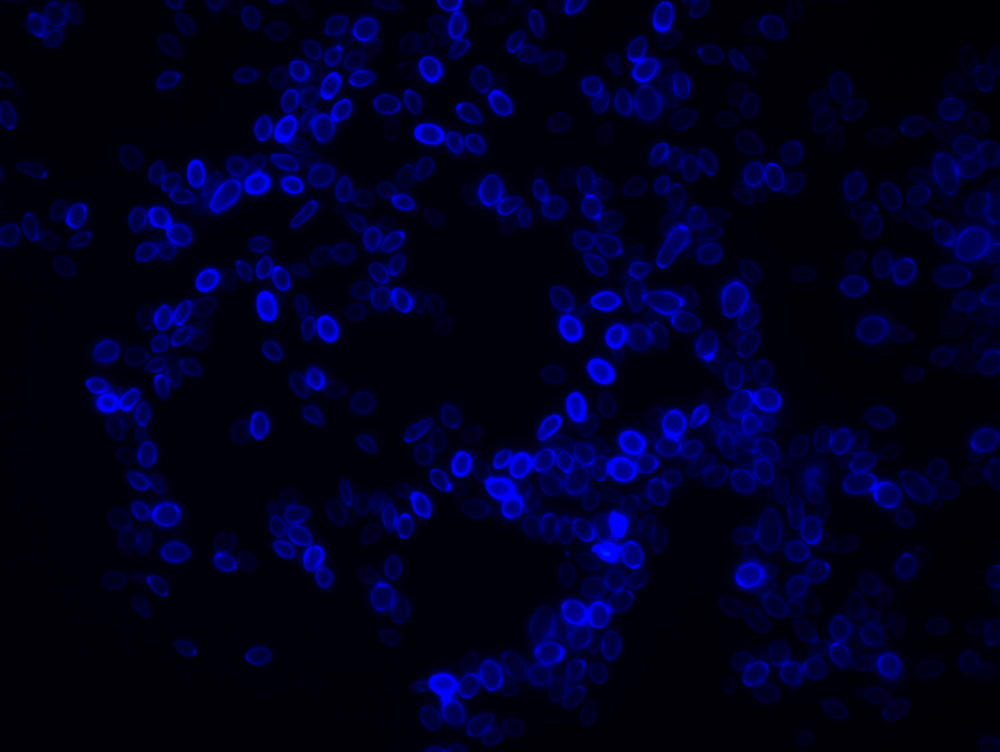 Candida auris under the microscope in the UAB Fungal Reference Lab.
Candida auris under the microscope in the UAB Fungal Reference Lab.Image courtesy Dr. Sixto Leal
The storm is spreading
But Alabama’s bad news is also good news in a world where fungi are becoming a global health threat. Most fungi cannot survive the 98.6-degree temperature of the human body, but a warming planet is changing that. And widespread use of industrial antifungals — sprayed on crops and mixed in with paint, among many other applications — is increasing resistance to the limited number of antifungal treatments on the market. Worldwide, fungal diseases kill more than 1.5 million people each year, and the number is rising.
 Peter G. Pappas, M.D.
Peter G. Pappas, M.D.
Illustration by Jody Potter | University RelationsAlabama’s climate and population, and UAB’s reputation, mean that patients here can be cared for by specialists such as Pappas and Sixto M. Leal Jr., M.D., Ph.D., an associate professor in the Department of Pathology whose hospital labs can track the spread of fungal infections like nothing else in the state. That gives Alabama an advantage as new fungi are on the march around the world.
The HBO hit “The Last of Us,” and the video game that inspired it, revolve around a fictional fungus-based apocalypse. Meanwhile, reality has contributed its own fungal supervillain: Candida auris. This treatment-resistant yeast, with a mortality rate of 60 percent, was first identified in 2009 in Japan and appeared in the United States in 2013. More than 2,377 people in the United States were infected with C. auris in 2022, according to the CDC — up from 53 in 2016.
“Most yeasts like to be in a moist environment — wet soil, pigeon droppings, the GI tract,” said Leal, who is director of ground zero for C. auris testing in the UAB health system: the Clinical Microbiology Lab for UAB Hospitals and the UAB Fungal Reference Lab. “They live within you, so you don’t have to worry about getting it from a door handle or sheets,” Leal said. “But C. auris can live outside the body, so it spreads. It can hang out in rooms and live on bedsheets.”
Alabama did not have a C. auris case until 2022, when it was identified by Leal’s lab. Since then, five more Alabama cases have been reported to the CDC’s database. So far, “all the patients with C. auris at UAB have been susceptible to micafungin, the first-line therapy for anyone in the ICU that you think may have fungus in the blood,” Leal said.
 Sixto M. Leal Jr., M.D., Ph.D.
Sixto M. Leal Jr., M.D., Ph.D.Illustration by Jody Potter | University Relations
Experts with national reputations
Leal’s labs, perhaps the best equipped in the state, can rapidly identify C. auris and thousands of other pathogens using two state-of-the-art MALDI-TOF machines. One is “the size of a Coke machine” and the other is a bit smaller. The test itself is high-tech, fast and cheap. “You start with a little slide that resembles an old Scantron bubble sheet,” Leal explained. “Instead of a No. 2 pencil, you fill in each bubble with a toothpick touched to a colony on an agar petri dish.” Inside the machine, “a laser zaps the organism and ionized protein fragments travel through a vacuum and strike a detector recording a spectrum that is unique for each species,” Leal said. “With MALDI, you can fill in that bubble in 10 seconds and it costs about 75 cents to get a result. It is way cheaper, faster and more accurate than biochemical panels, enabling us to rapidly identify thousands of fungi, molds and bacteria.”
“Since Sixto joined us [in 2018], it has allowed us to explore things in much more detail,” Pappas said. “We are able to do more rapid molecular-based diagnostics, which let you distinguish different strains of organisms. That allows us to explore and understand and deepen our fungal enterprise. He is pushing the envelope with respect to diagnostics that are more aggressive and emerging.”
Leal and Pappas have national reputations. When the magazine of the College of American Pathologists ran a major feature on how hospital labs were handling C. auris infections, it put Leal on the cover and quoted him extensively throughout. When the Wall Street Journal published a series of reports on C. auris and the fungal resistance to drugs, Pappas was quoted at the top of each article.
Another comment in one of those Wall Street Journal stories, from Tom Chiller, M.D., leader of the CDC’s Mycotic Diseases Branch, captures the urgency experts feel at the moment. “We desperately need new drugs,” Chiller said.
Pappas and Leal each have received major research awards recently for their fungal research.
In September, the Mycoses Study Group was awarded a five-year, $7.5 million U01 grant from the CDC, with Pappas as principal investigator. The grant will fund extensive study on the use of industrial antifungals and antifungal resistance nationwide.
Leal, who is the scientific director of UAB’s regional biocontainment facility, also has an active research program. This summer, Leal received a four-year, $2.97 million R01 grant from the National Institute of Allergy and Infectious Diseases to study the underlying mechanisms of COVID-associated fungal infections. “Approximately, 5 to 10 percent of individuals with severe COVID develop secondary mold infections, including COVID-associated pulmonary aspergillosis, or CAPA,” Leal said. “We are trying to understand how viral infection makes otherwise healthy individuals vulnerable to mold infection.”
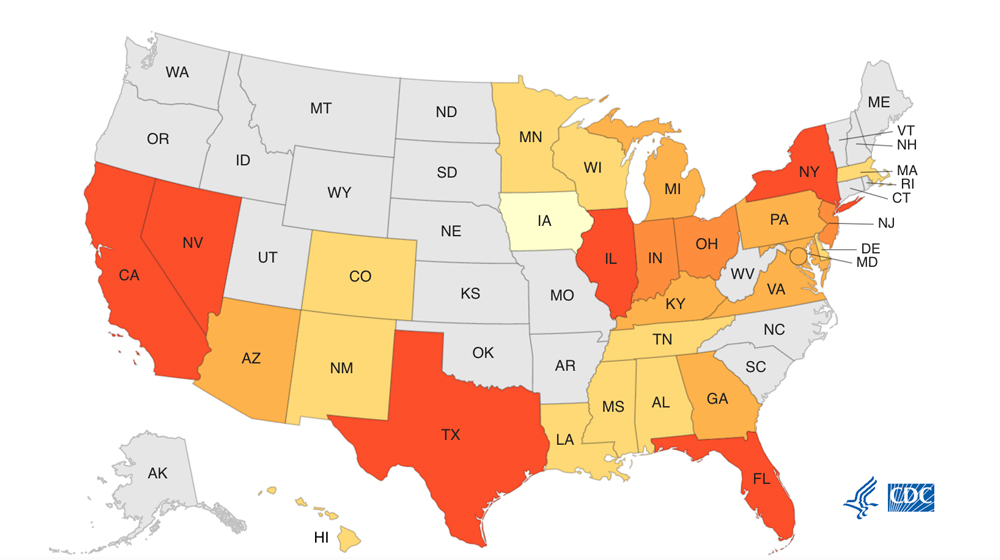 CDC tracking chart of Candida auris cases reported in 2022.
CDC tracking chart of Candida auris cases reported in 2022.
Testing new treatments
Thanks to UAB’s position in the Mycoses Study Group and Pappas’ reputation in the field, UAB investigators are helping to test most of the new antifungal drugs in development. Pappas was part of a group of investigators who published results from a Phase 2 study of one promising new treatment from Pfizer, Fosmanogepix, in May 2023.
Fosmanogepix is part of “a new class of drugs,” Pappas said. “Most antifungals work at either the cell wall, which is on the outside, or the plasma membrane right on the inside. Fosmanogepix interacts with anchor proteins that are directly involved in plasma membrane and cell wall synthesis. The important thing is that it is a different mechanism of action. There are relatively few drugs and few mechanisms of action for treating fungal diseases. Doctors have only a few choices, and that is one of the things that make fungi difficult to treat. The drugs you can use that are not super toxic are pretty limited.”
Story continues below image
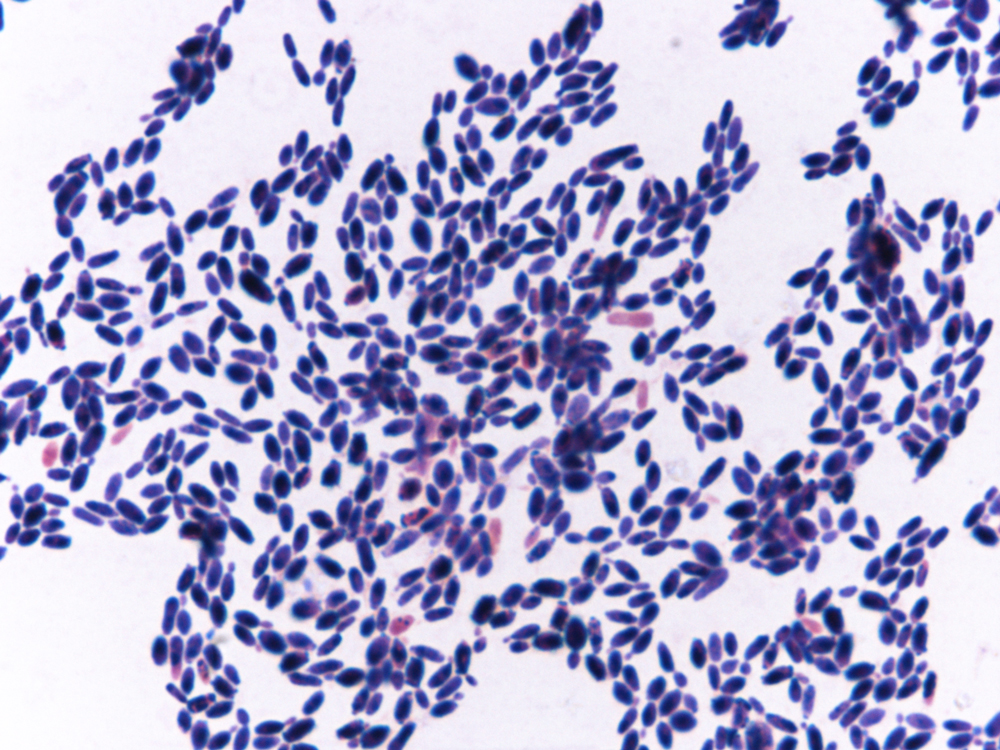 Another view of Candida auris from Dr. Leal's lab.
Another view of Candida auris from Dr. Leal's lab.
Image courtesy Dr. Sixto Leal
The benefit of having a new class of drugs “is it allows you to perhaps treat different fungi or treat certain fungi better,” Pappas said. “For instance, Fosmanogepix hits C. auris really hard. But there is another Candida species that it doesn’t hit at all.”
Pappas and UAB also are involved in trials for an oral drug called Ibrexafungerp (saying it, Pappas chuckles at the tongue-twisting name). Ibrexafungerp was approved by the Food and Drug Administration in 2021 to treat vaginal yeast infections, and experts want to know whether it can treat more severe diseases.
The UAB team also is involved in studying a next-generation drug called rezafungin given weekly as treatment or prevention of fungal infection in selected patients. The ReSTORE Phase 3 trial, published in The Lancet in January 2023, with Pappas as senior author, studied efficacy and safety outcomes of a weekly dose of rezafungin in patients with candidemia and invasive candidiasis, demonstrating similar efficacy to standard-of-care treatment for this condition.
Todd McCarty, M.D., associate professor in the Division of Infectious Diseases, is the principal investigator for the ReSPECT trial at UAB. The ReSPECT study evaluates once-weekly prophylactic treatment with rezafungin compared to daily standard of care for prevention of invasive fungal infections among high-risk patients receiving stem cell transplantation. “If it works,” this could eventually become the standard of care for high-risk patients, Pappas said. Pappas says he hopes to convince the young faculty member to focus on fungal research. Despite their recent higher profile, fungi still lag behind viruses and bacteria in research attention, Pappas says.
Why fungi, exactly?
So how did Pappas get into the fungus game? “I went to medical school at UAB,” and he came back after stints in Washington, Colorado and North Carolina, he said. “One of the people who hired me, Bill Dismukes, had a real interest in fungal infection. He steered me in that direction.” (William Dismukes, M.D., was the original principal investigator of the Mycoses Study Group “and quite a figure in clinical mycology,” Pappas said.) “There was so much of it [fungal disease] here and no one else was doing it, so I tried to fill the vacuum.”
Leal first became attracted to fungi because of the “unique host-pathogen battle — they try to kill you and you try to kill them,” he said. During his M.D./Ph.D. training, “people around the world were losing their eyes” due to a contact-lens-related global outbreak of antifungal-resistant mold infections, he said. Upon digging deeper, Leal realized that cornea mold infections were a huge global health issue causing blindness in more than 1.5 million people worldwide every year, particularly in neglected tropical communities within India, China and Africa. Leal established the first mouse model of this disease and worked in Tamil Nadu, India, to evaluate affected patients and the host immune response. “This experience brought me into medical mycology, and the field has fascinated me ever since,” he said.