 In a new paper, UAB clinicians and researchers explain how they use natural language processing to find patients who had unusual growths on their adrenal glands noted during imaging for another condition. They then contact these patients and connect them with UAB's dedicated Adrenal Gland Incidentaloma Clinic. This is the first paper to describe the combination of AI tools and a dedicated AGI clinic.The patients always start out seeking care for something else. They may have just experienced a heart attack, or been in a car accident, or have a possible chest infection. Alternatively, they may be getting a scan to monitor the progress of a cancerous tumor. The key is that the condition calls for cross-sectional imaging of the abdomen or an abdomen-adjacent area.
In a new paper, UAB clinicians and researchers explain how they use natural language processing to find patients who had unusual growths on their adrenal glands noted during imaging for another condition. They then contact these patients and connect them with UAB's dedicated Adrenal Gland Incidentaloma Clinic. This is the first paper to describe the combination of AI tools and a dedicated AGI clinic.The patients always start out seeking care for something else. They may have just experienced a heart attack, or been in a car accident, or have a possible chest infection. Alternatively, they may be getting a scan to monitor the progress of a cancerous tumor. The key is that the condition calls for cross-sectional imaging of the abdomen or an abdomen-adjacent area.
While reading the image, a radiologist notes something unusual on the patient’s adrenal glands — small, triangle-shaped organs that sit near the top of the kidneys. The mass or nodule is called an adrenal gland incidentaloma, because it was found while looking for something else. It is unlikely to be cancerous. (Adrenal gland cancers are rare.) But in most cases, it is something to be investigated. The adrenal glands produce powerful hormones such as cortisol, adrenaline, aldosterone and some sex hormones. The adrenal gland incidentaloma, or AGI, could be pumping excess hormones into the patient’s body, raising their blood pressure, and increasing their risk of stroke, high blood pressure, diabetes complications, bone disease and other serious problems.
“Not everyone with high blood pressure or diabetes has an adrenal nodule; but for people who do have this hormone oversecretion, to think that an outpatient operation can cure your high blood pressure or improve your diabetes is amazing,” said Brenessa Lindeman, M.D., associate professor in the UAB Department of Surgery in the Heersink School of Medicine and medical director of UAB’s Adrenal Gland Incidentaloma Clinic, which was launched in 2022.
A worldwide problem
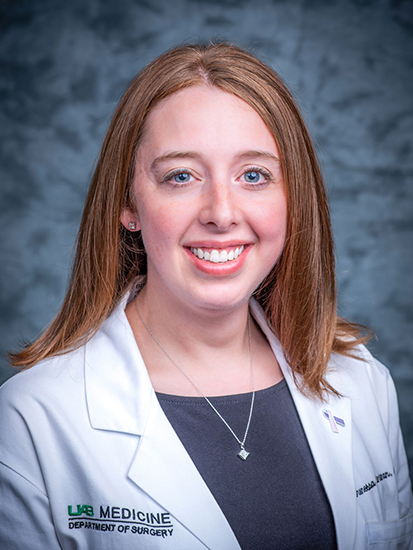 “Not everyone with high blood pressure or diabetes has an adrenal nodule; but for people who do have this hormone oversecretion, to think that an outpatient operation can cure your high blood pressure or improve your diabetes is amazing,” said Brenessa Lindeman, M.D., senior author of the paper and medical director of the AGI Clinic.AGIs will be found on about 5 percent of all abdominal scans, and up to 10 percent of scans in patients over the age of 65, or in patients with hypertension, diabetes and obesity. A quarter of the AGIs, according to estimates, will be biochemically active or be cancerous. This is why guidelines from a number of medical societies, including the American Association of Endocrine Surgeons, call for any AGI that is 1cm (less than half an inch) in size or larger to trigger a biochemical evaluation (usually a few blood tests) to check for abnormal hormone levels. But that happens in only 18 percent of patients with AGIs, according to a recent systematic review.
“Not everyone with high blood pressure or diabetes has an adrenal nodule; but for people who do have this hormone oversecretion, to think that an outpatient operation can cure your high blood pressure or improve your diabetes is amazing,” said Brenessa Lindeman, M.D., senior author of the paper and medical director of the AGI Clinic.AGIs will be found on about 5 percent of all abdominal scans, and up to 10 percent of scans in patients over the age of 65, or in patients with hypertension, diabetes and obesity. A quarter of the AGIs, according to estimates, will be biochemically active or be cancerous. This is why guidelines from a number of medical societies, including the American Association of Endocrine Surgeons, call for any AGI that is 1cm (less than half an inch) in size or larger to trigger a biochemical evaluation (usually a few blood tests) to check for abnormal hormone levels. But that happens in only 18 percent of patients with AGIs, according to a recent systematic review.
“Lots of these scans are conducted in the trauma setting,” Lindeman said. “If you have been in a car accident, nobody cares about an adrenal nodule right now, and by the time you are released from the hospital three weeks later, maybe people have forgotten.”
Lindeman is senior author of a paper published in the World Journal of Surgery in December 2024 that presents a solution to this pressing global problem. Using a blend of computer science, technology and human persistence, the authors have developed a sustainable method to find and engage with patients who have AGIs and connect them to care. The technology side relies on natural language processing, or NLP, “an artificial intelligence tool used to understand human language in a computational setting through the recognition of certain words and phrases,” the authors explain. The human side comes from a dedicated nurse practitioner who contacts the patients identified by NLP, tells them about the AGI Clinic and guides them through the evaluation process. Both approaches have been tried before, Lindeman points out; but this is the first paper to describe what happens when they are combined.
Success for AGI Clinic model
In one year, from March 2022 to February 2023, the UAB team identified 899 patients and invited them to the AGI Clinic; 382 patients were seen in the clinic, and 322 were included in the intervention cohort. Of those, 99 percent underwent biochemical testing and 40 percent underwent adrenal-specific imaging. Sixteen patients (5 percent) underwent adrenalectomy — a surgical procedure to remove the AGI. “In this report, we have demonstrated that natural language processing can be successfully utilized to search thousands of radiology reports to efficiently identify patients with AGIs,” the authors write. “An NLP-informed AGI clinic is a viable approach to efficiently improve the system-wide quality of care for patients with AGIs.”
 The same techniques used to identify AGIs are being applied to other incidental findings. "We are developing programs to identify these incidental findings and establishing the clinical partnerships to connect patients to appropriate follow-up,” said study co-author Srini Tridandapani, Ph.D., M.D., interim chair of the Department of Radiology.The researchers are expanding their technique to identify other incidental findings on radiology imaging that are often lost to follow-up. “We have taken these algorithms and applied them to abdominal aortic aneurysms, incidental lung nodules and pancreatic cysts,” Lindeman said.
The same techniques used to identify AGIs are being applied to other incidental findings. "We are developing programs to identify these incidental findings and establishing the clinical partnerships to connect patients to appropriate follow-up,” said study co-author Srini Tridandapani, Ph.D., M.D., interim chair of the Department of Radiology.The researchers are expanding their technique to identify other incidental findings on radiology imaging that are often lost to follow-up. “We have taken these algorithms and applied them to abdominal aortic aneurysms, incidental lung nodules and pancreatic cysts,” Lindeman said.
The Department of Radiology is “really excited about the possibilities we can get to,” said paper co-author Srini Tridandapani, Ph.D., M.D., MBA, professor and interim department chair. “In some ways, we are changing the way we practice based on these outcomes. We are developing programs to identify these incidental findings and establishing the clinical partnerships to connect patients to appropriate follow-up.”
“With their focus appropriately being on acute, life-threatening or chronic medical conditions, neither EM [emergency medicine] physicians nor PCPs [primary care physicians] are ideally suited to workup and follow AGIs long term,” the authors of the paper write. “We believe that an ideal use-case for NLP is as an adjunct in PCP offices and emergency departments in identifying patients with AGIs or other chronic incidental findings (e.g., lung or liver lesions) and then automatically enrolling them in a dedicated specialty clinic.”
A raspberry-shaped dilemma
Under a microscope, an AGI is a ball of cells that looks like a raspberry, Lindeman said. “And then each of those cells can secrete hormones.” To a radiologist, the AGI looks like a dilemma.
Here’s why: The radiologist’s observation of an adrenal gland growth — along with the more urgent matters that were the reason for the imaging in the first place, and anything else that the radiologist notes in the scan — gets included in the findings section of the radiologist’s report. “Then there is the impression section, which is the synthesis of all the findings,” said Tridandapani, who is also vice chair for Imaging Informatics in the Department of Radiology. “We try not to put a lot of clutter in the impression because that is not what the ED doctor needs right then. They are just trying to make a decision about whether to admit the patient to the hospital or not.”
A note will go in the patient’s file to make an appointment for follow-up in six months or a year, but laws against self-referral prevent radiologists from contacting patients directly to set up those appointments. “It’s not something you have to deal with immediately, so they can get lost,” Tridandapani said.
Finding patients with NLP
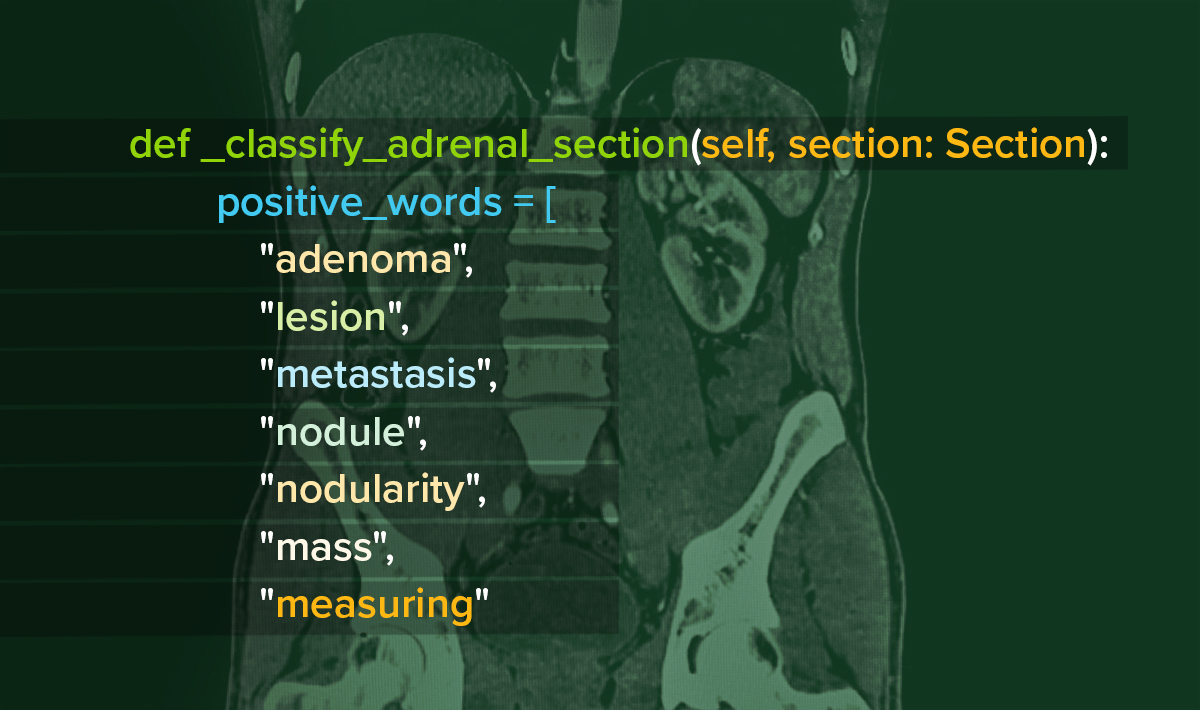
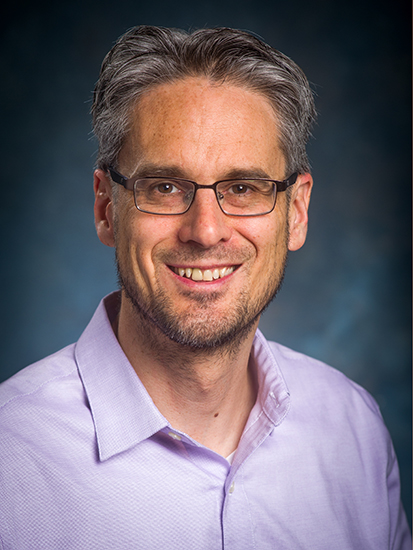 To identify incidental findings mentioned in radiology reports, the researchers use a tool created by study co-author John Osborne, Ph.D. “My tool pulls data from the electronic health record and uses a combination of keywords and structured data to identify patients,” Osborne said.To find these patients, whose care may have occurred in clinics across the UAB Health System, the researchers leveraged a system built by paper co-author John Osborne, Ph.D., an associate professor in the Department of Biomedical Informatics and Data Science who also has an appointment in the Department of Computer Science in the UAB College of Arts and Sciences. While working as a researcher in UAB’s Center for Clinical and Translational Science, or CCTS, in the early 2010s, Osborne developed a program that used NLP to find patients with reportable cancers in UAB’s electronic health records system. In 2016, he received a grant from the UAB Health Services Foundation’s General Endowment Fund to expand that into a general-purpose system called PheDRS, or the Phenotype Detection Registry System. “My tool pulls data from the electronic health record and uses a combination of keywords and structured data to identify patients,” Osborne said. It has been used in a wide range of projects, identifying patients with lung nodules, COPD “and many other applications,” he said.
To identify incidental findings mentioned in radiology reports, the researchers use a tool created by study co-author John Osborne, Ph.D. “My tool pulls data from the electronic health record and uses a combination of keywords and structured data to identify patients,” Osborne said.To find these patients, whose care may have occurred in clinics across the UAB Health System, the researchers leveraged a system built by paper co-author John Osborne, Ph.D., an associate professor in the Department of Biomedical Informatics and Data Science who also has an appointment in the Department of Computer Science in the UAB College of Arts and Sciences. While working as a researcher in UAB’s Center for Clinical and Translational Science, or CCTS, in the early 2010s, Osborne developed a program that used NLP to find patients with reportable cancers in UAB’s electronic health records system. In 2016, he received a grant from the UAB Health Services Foundation’s General Endowment Fund to expand that into a general-purpose system called PheDRS, or the Phenotype Detection Registry System. “My tool pulls data from the electronic health record and uses a combination of keywords and structured data to identify patients,” Osborne said. It has been used in a wide range of projects, identifying patients with lung nodules, COPD “and many other applications,” he said.
A somewhat analogous system managed by the UAB CCTS, known as i2b2, or Informatics for Integrating Biology and the Bedside, allows researchers to gather anonymized data. “The distinction is that PheDRS is for interactive, daily updates,” Osborne said. He and his lab team, including programmer Micah Cochran, meet with collaborators to determine their needs. Straightforward projects may not require much adaptation of Osborne’s existing algorithms. “If they want to use some new NLP, which often requires machine learning, we can fund that through a grant,” Osborne said.
Connecting with patients
Other researchers have used NLP to identify incidental findings that would be worth following up, “but then it becomes overwhelming to manage them,” Lindeman said. The crucial innovation responsible for the success of the AGI Clinic, she says, was to combine the NLP with dedicated personnel: Nurse Practitioner Haleigh Negrete, CRNP. “This is all she does, which has allowed her to build incredible expertise around adrenal pathophysiology,” Lindeman said.
When Osborne’s algorithm flags a patient, their name appears on Negrete’s list for contact. During the study period, she would call each patient, explain about the clinic and the patient’s abnormal imaging result and ask if they would be willing to come in to follow up on the finding. Patient reactions have been “a mixed bag,” Negrete said. “Some people are grateful, others are hesitant, and others are fearful. But we found that, if we could get them in the door to our clinic, we could put those fears to rest.”
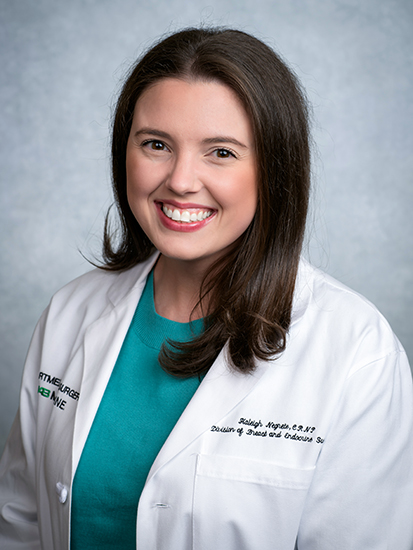 Nurse Practitioner (and study co-author) Haleigh Negrete, CRNP, connects with patients to let them know about their findings and about the AGI Clinic. “I do a lot of education, as most people don’t know what an adrenal gland is or what it makes," Negrete said. "I explain the long-term effects of these hormones, including stroke, diabetes, high blood pressure and bone disease.”Not all of the visits require a trip to UAB. “We do a mixture of in-person and telehealth since a lot of our visits are communication-based,” Negrete said. “I do a lot of education, as most people don’t know what an adrenal gland is or what it makes. I explain the long-term effects of these hormones, including stroke, diabetes, high blood pressure and bone disease.” The possible consequences of their bodies’ making too many adrenal hormones “usually motivates patients to complete the sometimes-tedious workup” that is involved, Negrete added.
Nurse Practitioner (and study co-author) Haleigh Negrete, CRNP, connects with patients to let them know about their findings and about the AGI Clinic. “I do a lot of education, as most people don’t know what an adrenal gland is or what it makes," Negrete said. "I explain the long-term effects of these hormones, including stroke, diabetes, high blood pressure and bone disease.”Not all of the visits require a trip to UAB. “We do a mixture of in-person and telehealth since a lot of our visits are communication-based,” Negrete said. “I do a lot of education, as most people don’t know what an adrenal gland is or what it makes. I explain the long-term effects of these hormones, including stroke, diabetes, high blood pressure and bone disease.” The possible consequences of their bodies’ making too many adrenal hormones “usually motivates patients to complete the sometimes-tedious workup” that is involved, Negrete added.
When an adrenal nodule is overproducing hormones, minimally invasive outpatient surgery can fix the issue, Lindeman says. “When I talk with patients, I tell them it is a lot like having your gallbladder taken out,” she said.
When patients are not good candidates for surgery, or do not want surgery, medical management is possible in many cases, Lindeman says. But when studies have compared surgical management of adrenal hormone hypersecretion with attempted medical management, “the surgery group always does better,” she pointed out.
In many cases, testing will show that the AGI is not producing hormones or having any other ill effects, giving patients, and their caregivers, peace of mind. As the clinic has become more well known, Negrete says she is receiving more and more referrals from doctors directly, even before the patients are flagged by Osborne’s algorithms. “Once they realized we were out there, they started calling,” Negrete said. “That is what we want. The heart of the clinic is just making sure people get follow-up.”
In addition to Lindeman, Tridandapani, Osborne and Negrete, authors of the paper, “A natural language processing-informed adrenal gland incidentaloma clinic improves guideline-based care,” are C. Corbin Frye, M.D., Ramsha Akhund, M.D., Mohammad Murcy, M. Chandler McLeod, Ph.D., Andrea Gillis, M.D., Jessica Fazendin, M.D., and Herbert Chen, M.D., of the UAB Department of Surgery; Lillie Grace Veazey of the Heersink School of Medicine; Micah Cochran of the UAB Department of Biomedical Informatics and Data Science; and Steven Rothenberg, M.D., of the UAB Department of Radiology.