 |
Gorgas Case 2002-04 |
 |
|
The following case was seen in the Tropical Disease Unit at Cayetano Heredia Hospital by Gorgas Course participants.

 History: 43 year-old male initially noted non-tender swelling beginning at the great toe 30 years earlier. Swelling has progressed gradually to the nodular lesion shown in the bottom image. 3 years ago sinus tracts and drainage of purulent material with bits of black granular material began which have not responded to antibacterials. No fever, weight loss, or respiratory symptoms. Otherwise well.
Epidemiology: Rice farmer born in Piura in the north of Perú but has lived most of his life on a farm near Chiclayo, a coastal region of the country. No TB exposure. Physical Examination: Afebrile. Normal exam except for foot lesions draining black granular material as shown in the digital images (indicated by arrows, bottom Image). Laboratory Examination: Normal CBC, liver, and renal function; normal chest x-ray. X-ray of foot shows mild periostitis in area of lesion with questionable changes consistent with chronic osteomyelitis.
|
|
Diagnosis: Madura foot due to Madurella mycetomatis.
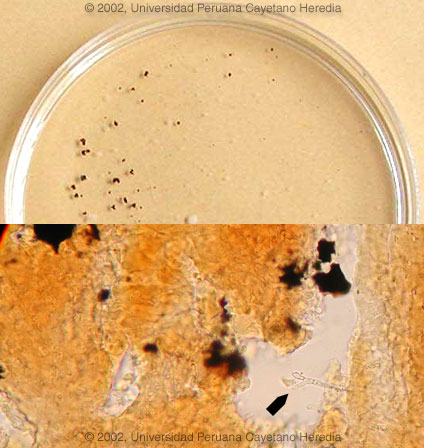
 Discussion: The black granules (so called sulphur granules) in the sinus tract drainage [top Image] were examined microscopically in a KOH preparation, and in addition to the characteristic granules, hyphal forms diagnostic of Madurella mycetomatis were seen [arrow, bottom Image]. Culture of the material is pending, as usually Madurella takes a month or more to grow. Excisional biopsy or invasive cultures of the sinus tracts are not usually necessary for diagnosis of madura foot as the sulfur granules usually come to the surface even if not on a daily basis. The main and important differential diagnosises in this case are TB, botryomycosis (chronic staphylococcal infection) [see Gorgas Case 2003-04], actinomycosis [see Gorgas Case 2001-09], other causes of chronic bacterial osteomyelitis, and malignancy. Madura foot is a common subcutaneous mycosis in the tropics and is caused by a wide variety of fungal organisms. Madura foot typically presents in a similar way to this patient, with a small local tumor slowly progressing over years to more widespread destruction of subcutaneous tissue and bone while sparing nerve and vasculature. Etiologic agents of maduramycosis are divided into 2 groups:
Maduramycosis is most common in Africa, Central and South America, and the Far East. Most cases occur in tropical latitudes between 15 degrees South and 30 degrees North in humid moist environments. The organisms have been isolated from soil as well as from plant thorns. In contrast to mycetoma due to bacterial agents of actinomycetoma, which are responsive to anti-bacterial drugs or combinations of antibacterial agents, madura foot has been characterized as being poorly responsive to medical therapy, and aggressive surgery or amputation is commonly recommended. Although randomized controlled trials are not available, recent consensus from experts in highly endemic areas of Africa and the Americas indicates that 6 to 12 months of ketoconazole is very often successful in improving the lesions, even if complete cure is not achieved. Newer azole agents seem to be less effective in limited open trials. In tropical countries, amputation or highly destructive excisional procedures in impoverished rural residents usually carriers a poor prognosis for rehabilitation and ongoing complications. Prosethetic appliances are not available. Because the infection does not disseminate and is non-painful, surgery should be used only as a last resort with widespread disease, weighing the benefits versus the above-mentioned adverse aspects of this kind of surgery in certain settings. Less than extensive disease can often be observed for several years even if drug therapy is not available.
|