 |
Gorgas Case 2003-04 |
 |
|
The patient was seen by the Gorgas Course participants on the 36-bed inpatient ward of the Tropical Medicine Institute.
 History: Patient initially presented as a 16 year-old 2 years prior to the present admission. At that time she had a 1-year evolution of a red papule over a pre-existing long-standing traumatic scar. The papule began to suppurate and drain yellowish material through multiple sinus tracts. A surgical resection followed by oral antibiotics caused a temporary remission, but the patient presented a few weeks later with headache and drainage of purulent material containing granular material. No history of past illnesses.
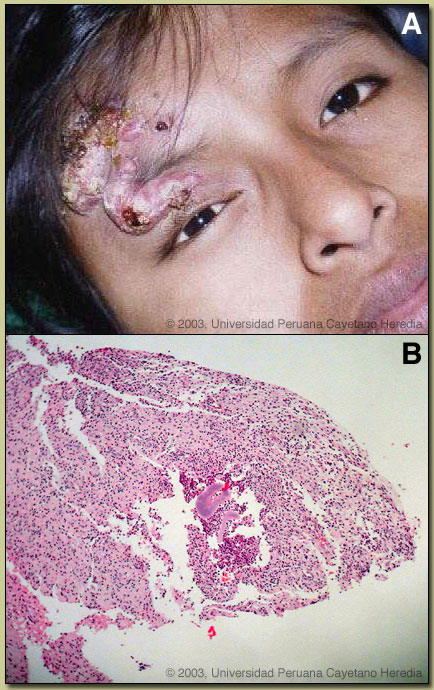
Epidemiology: Born and living in the high jungles of central Perú for her whole life. No contact with TB or persons with febrile illness. Physical Examination: (at the initial admission) Afebrile. Normal except for the lesion shown in the image at right [panel A]. Laboratory Examination: (at the initial admission) Hct 36. WBC 6.2 with 58 neutrophils and no left shift. Liver function tests and electrolytes normal. HIV-1 and HTLV-1 negative. CXR normal. H&E stained biopsy of the forehead lesion is shown [panel B].
|
|
Diagnosis: Botryomycosis (bacterial pseudomycosis) due to Staphylococcus aureus.

 Discussion: Botryomycosis is an uncommon chronic bacterial infection with a global distribution in the tropics and non-tropics. The disease is characterized by the presence of granules containing a central mass of bacteria within an area of pus. In the tropics, clinically and histologically, botryomycosis can mimic both mycetoma [see Gorgas Case 2002-04] and actinomycosis [see Gorgas Case 2001-09]. Both of these are much more frequent infections and also present with suppurative draining lesions with granules in the pus. Had the purulent lesion presented to us without the granule formation, other possible diagnoses would have included TB, sporotrichosis, malignancy or chronic osteomyelitis. Other uncommon subcutaneous mycoses include chromomycosis, and lobomycosis (phaeohyphomycosis). Up to one-third of cases of botryomycosis present with only deep visceral involvement, usually in debilitated patients. Grossly the granules of botryomycosis are yellowish-white and 1-3 mm in diameter. The biopsy included in the case presentation shows a large granule in the center together with scattered micro-abscesses with pus and sinuses (because of pus moving between micro-abscesses). A high power view close-up of the granule [2nd image, panel A] shows an eosinophilic border (so-called Splendore-Hoeppli phenomenon) and blue dots in the center that are aggregates of cocci-form bacteria. If this were a mycetoma in Perú, one would expect to see distinct hyphae inside the black granules characteristic of Madurella mycetomatis or related fungus. In actinomycosis branching filamentous acid-fast bacteria would be expected. Culture of the wound grew pure Staphylococcus aureus sensitive to oxacillin. Until Staphylococcus aureus was cultured from lesions in 1919, botryomycosis was believed to be fungal in nature, hence the name. The infection is uncommon but no specific incidence data is available. The literature consists of about 150 case reports and no large case series but we have seen at least 3 cases in recent years suggesting it is not as rare as the numbers in the published literature. Staphylococcus aureus causes the majority of infections, followed by Pseudomonas aeruginosa and then a long list of other bacteria. Pathogenesis is not clear but limited animal work suggests that it is related to bacterial strain, innoculum of bacteria, and perhaps host immune response. The frequent findings of intracellular bacteria suggest a host immune defect. Most of the individual case reports have been in individuals with impaired T-cell immunity of one sort or another, including HIV infection, but again there are no systematic incidence studies. One of the recent cases we have seen was HTLV-1 positive. Our patient has had a protracted and chronic course. Initial CT scan 2 years ago did show osteomyelitis of the frontal bone, subdural empyema, and cerebritis. She was treated with IV oxacillin then clindamycin for the first month, then oral clindamycin for several months until a surgical debridement of skin, bone, and brain was performed. She looked well after 1 month of post-operative IV therapy. She presented with a relapse 6 months ago and a repeat CT scan [2nd image, panel B] showed temporal and frontal osteomyelitis. At debridement this time, oxacillin-resistant Staphylococcus aureus was cultured. She has been treated since with IV vancomycin but we have just ascertained that she became pregnant on a visit home during Christmas and will need to switch to clindamycin for now. The lesion is presently healing [2nd image; panel C]. In the absence of any literature, we will continue IV treatment for at least 1 year since the last debridement.
|