| 2009 Case #5 |  |
|
| Diagnosis: Old world cutaneous leishmaniasis due to Leishmania major. |
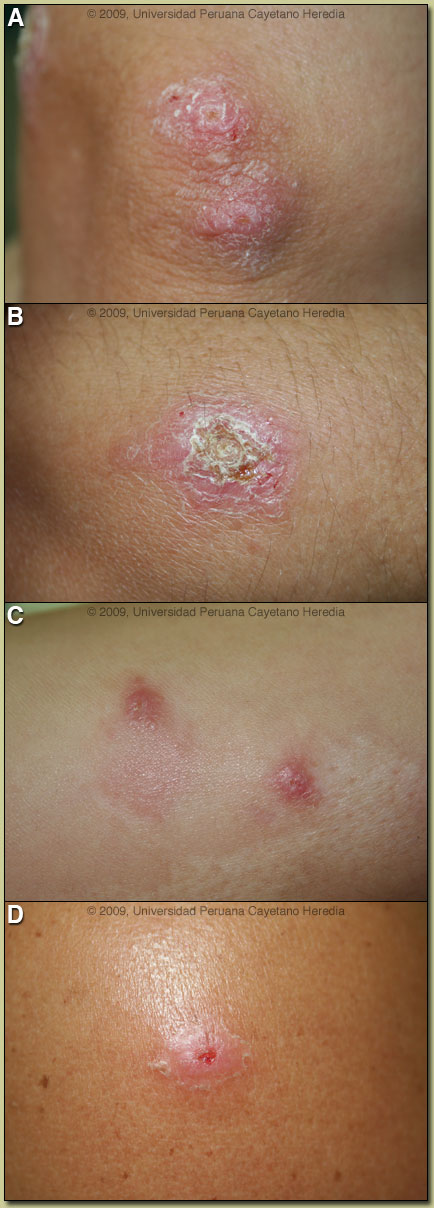
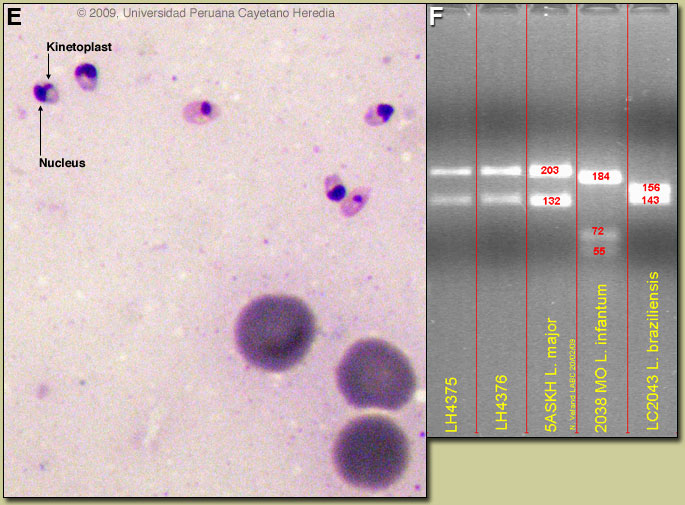 Discussion: A giemsa stained scraping from the border of a lesion showed multiple amastigote stages of leishmania [Image E: arrows show organism with nucleus and smaller darkly staining kinetoplast]. No growth was seen in cultures incubated in biphasic NNN media from the scrapings, but culture of a tissue punch biopsy yielded sufficient numbers of organisms for speciation by ITS1-PCR amplification. Image F lanes 4375 and 4376 show DNA fragments aligning with the old world cutaneous species L. major and not with L. braziliensis or L. infantum. A Moroccan L. tropica control was not run but would have generated an unmistakably different banding pattern [Emerg Infect Dis. 2007 Sep;13(9):1358-60]. Discussion: A giemsa stained scraping from the border of a lesion showed multiple amastigote stages of leishmania [Image E: arrows show organism with nucleus and smaller darkly staining kinetoplast]. No growth was seen in cultures incubated in biphasic NNN media from the scrapings, but culture of a tissue punch biopsy yielded sufficient numbers of organisms for speciation by ITS1-PCR amplification. Image F lanes 4375 and 4376 show DNA fragments aligning with the old world cutaneous species L. major and not with L. braziliensis or L. infantum. A Moroccan L. tropica control was not run but would have generated an unmistakably different banding pattern [Emerg Infect Dis. 2007 Sep;13(9):1358-60].
Old world cutaneous leishmaniasis is almost always caused by either L. major or L. tropica and is transmitted by Phlebotimus species sandflies; P. papatasi (L. major) and P. sergenti (L. tropica). In the Mediterranean basin certain variants of L. infantum, normally an agent of visceral leishmaniasis can cause purely cutaneous disease. A map of leishmania distribution in Morocco is available [Emerg Infect Dis. 2007 Sep;13(9):1358-60]. Several other species occur in localized distributions and cause a small percentage of old world cases. L. major is a zoonosis that most typically causes mild and often self-limited disease in North Africa and the Middle East. L. major from central Asia, including Afghanistan, seems to be more aggressive. Incubation period is normally about a month and lesions begin as plaques or nodules, eventually progressing to so-called wet ulcers. Systemic disease does not occur. L. tropica is anthroponotic and mostly causes dry nodular lesions. Sporadic jumps of L. tropica from desert gerbils living in rocky outcrops to locals who live nearby may then set up the cycle of human to human transmission; this patient only had exposure in sandy dune areas with no rocky outcroppings. Gorgas Cases of the Week normally report on endemic diseases of Perú but this case illustrates the importance of a good travel history in any setting. If the disease had been acquired in South America, where the vector is the Lutzomyia sandfly, it would have been important to distinguish Leishmania species that cause only cutaneous disease from those such as L. braziliensis that causes mucocutaneous disease. Both cause initial skin ulcers, but with mucocutaneous species, from months to years after treatment or healing of the painless skin ulcers, severe destructive recurrence may occur in the mucosal surfaces of the naso and oropharynx. Other considerations for these skin lesions had they been acquired in Perú would be spororichosis, atypical mycobacteria especially M. marinum, TB, nocardiosis, or psoriasis. There are multiple treatment options for old world disease, including no intervention in cases of single lesions in non-cosmetically sensitive areas, which will often self-heal. For small lesions local infiltration with pentavalent antimonials is utilized in many countries. Other local treatments such as ointments (e.g., paromomycin), diathermy, laser, and radiotherapy are often used but relatively poorly studied. For larger lesions systemic antimony may be used, and some success with fluconazole for L. major has been reported [N Engl J Med. 2002 Mar 21;346(12):891-5]. Amphotericin has not been properly studied for use in old world cutaneous leishmaniasis but many experienced clinicians in high resource environments would prefer liposomal amphotericin B over antimony if parenteral therapy were needed. More recently, miltefosine, a new oral agent that has revolutionized the treatment of visceral leishmaniasis, has been studied in a number of cutaneous leishmania species with varied success. Large blinded, well-controlled trials have not yet been done but 26/32 Iranian patients with L. major were cured with miltefosine [Acta Tropica 2007 Jul;103(1):33-40]. Because of the ease of oral administration, we elected a trial of oral miltefosine in this patient. The patient did not tolerate (gastrointestinal side effects as often occurs) the usual dosage of 2.5 mg/kg up to 150 mg/day in 3 divided doses for 4 weeks. She received 100 mg/day for 6 weeks instead, with the results shown in Image G, which shows the lesions prior to treatment, after 2 weeks of treatment, and after 6 weeks. We would like to thank 1) Nicolas Veland and Jorge Arevalo of the IMT Molecular Epidemiology Unit for the PCR analysis, and 2) Dr. Alan Magill, Gorgas Course Visiting Professor from the Walter Reed Army Institute of Research for consultation and discussion on the case.
|