 |
Gorgas Case 2018-01 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. For the 18th consecutive year, we are pleased to share interesting cases seen by the participants that week during the February/March course offerings. Presently the 9-week Gorgas Course in Clinical Tropical Medicine is in session. New cases will be sent by e-mail every Tuesday/Wednesday for the next 9 weeks. Each case includes a brief history and digital images pertinent to the case. A link to the actual diagnosis and a brief discussion follow.
Carlos Seas and German Henostroza
Course Directors |
|
The following case was seen on the Inpatient Ward of Cayetano Heredia Hospital in Lima by the 2018 Gorgas Course participants.
 History: 26-year-old MSM patient came to the emergency department complaining of two-month history of productive cough, fever, night sweats, dyspnea, weight loss of 10Kg in the last month, asthenia, diarrhea, and mild lower gastrointestinal bleeding (blood spots on his underwear). One week prior to admission the patient noticed a painless ulcerative lesion on the sacral region.
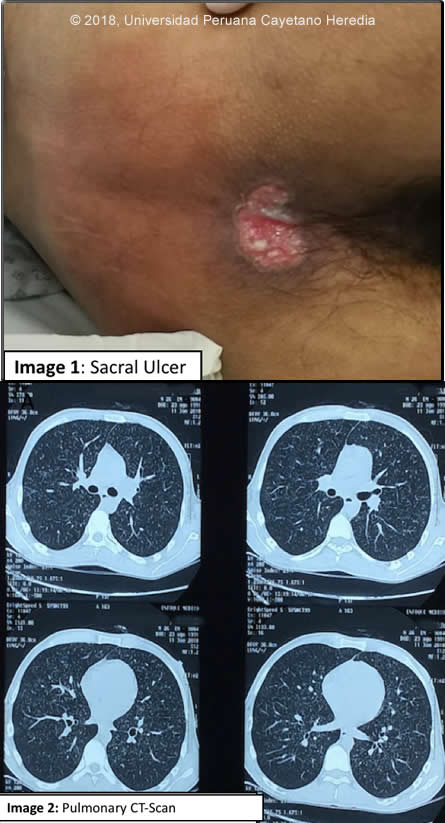
Past Medical History: Diagnosed in 2015 with HIV, (CD4=293 cells/mm3; viral load= 462,981 copies/ml. HAART (with zidovudine, lamivudine and efavirenz) was taken irregularly and stopped the medications two months ago with (CD4=18 cells/mm3; viral load=905,000 copies/ml. Epidemiology: Born in Pucallpa (jungle), moved to Ancash (highlands), at the age of 6 and has been living in Lima for the past 10 years. No known TB contact. Denies alcohol or drug consumption. Physical Examination: Pulse: 110; respirations: 28 SatO2:96% on 2l/min O2; BP: 102/61 mmHg; T:39,5C Patient in obvious respiratory distress. Skin: Pallor ++/+++, non-painful sacral ulcer 3x5cm with regular borders. (Image 1). Bilateral cervical lymphadenopathy. Chest: no rales in both lungs. Abdomen: normal bowel sounds, soft, non-tender, non-distended. No hepatosplenomegaly. Laboratory: Hemoglobin: 7.9 g/dl;, Hematocrit: 24%, WBC: 1,200; neutrophils:78%. Platelets: 95,000. Glucose: 106 mg/dl, Creatinine: 0.6 mg/dl. Alkaline Phosphatase: 1023 IU/l (N<126); LDH: 395 U/L (N=313-619); beta2 microglobulin: 3113 ng/ml (900-2700) Sputum AFB: negative x 3, culture pending. CT scan of the chest is shown (Image 2).
UPCH Case Editors: Carlos Seas, Course Director / Karen Luhmann, Associate Coordinator UAB Case Editor: David O. Freedman, Course Director Emeritus / German Henostroza, Course Director |
|
Diagnosis: Progressive disseminated histoplasmosis (PDH) due to Histoplasma capsulatum
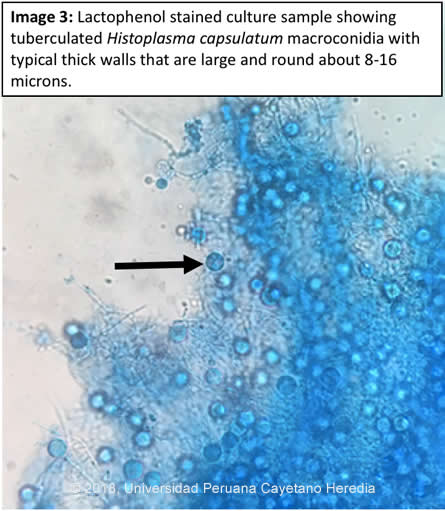
 Discussion: Histoplasma capsulatum was isolated from bone marrow culture. Image 3 shows diagnostic macroconidia with tuberculated typical thick walls that are large and round about 8-16 microns. Definitive diagnosis in these cases is made by fungal isolation (from bone marrow, blood or tissue samples including lymph nodes, skin or oral lesions) as a gold standard. Cultures are positive in about 75% of patients (AJTMH 2013;89:937). Urinary histoplasma antigen is very useful (97% sensitivity) but usually not available in developing countries. Direct observation of yeast cells from blood samples has low sensitivity (10%), better results are obtained from bone marrow samples. H. capsulatum is a dimorphic endemic fungus of worldwide distribution but is most common in North America and Latin America. In highly endemic areas more than 80% of persons are infected by age 20, often sub-clinically. Bats, which often live in caves, are frequently infected. Acquisition is inhalational with principal sites of disease in lungs, lymph nodes, liver, spleen, bone marrow, adrenals and the GI tract. In normal hosts, a self-limited pulmonary infection with mediastinal adenopathy is most common, but opportunistic disseminated infections in patients with depressed immunity, especially those with AIDS, is frequent. Endemic areas are the Mississippi, Ohio and St. Lawrence valleys in the USA, the Caribbean, Mexico and Latin America, South East Asia and Africa. Histoplasmosis is endemic in Latin America including Peru, the fungus is predominantly found in jungle areas. The reported incidence among advanced HIV-infected patients varies from 8% in Panama to 42% in French Guyana, being the first or second opportunist infection in these patients (AIDS 2016;30:167). A necropsy study of 16 patients who died with advanced AIDS in Lima, Peru found that 3 (19%) had disseminated histoplasmosis (Pathol Res Pract 2006;202:767). Exogenous acquisition or reactivation of a latent foci, as in this case are the modes of acquisition. Histoplasmosis is the most common endemic mycosis among HIV-infected patients. Progressive disseminated histoplasmosis (PDH) as demonstrated by this patient is the most common manifestation of histoplasmosis in AIDS patients. The Chest CT scan (Image 2) showed an interstitial infiltrate mainly composed of micronodules compatible with a milliary pattern. The differential diagnosis of these CT findings in a patient with HIV includes TB, PCP, penicilliosis (found mainly in Southeast Asia) and lymphoma. The differential diagnosis of the skin lesions in this patient includes herpes simplex infection, tuberculosis, paracoccidioidomycosis and cancer. PDH may be the first manifestation of advanced AIDS in endemic areas, a study among 89 patients with advanced AIDS in Colombia found 45 (51%) with PDH (AJTMH 2016;95:918); interestingly, 35% had TB as well. Predictors of PDH were significant weight loss, hepato or splenomegaly, skin lesions and hematologic abnormalities (mainly pancytopenia), all of them seen in this patient. Pulmonary involvement is seen in about 50-70% with non-specific manifestations (dry cough, chest pain, dyspnea); 50-70% of patients have abnormal radiologic findings; diffuse interstitial infiltrates or reticulonodular infiltrates are the most common abnormal findings. PDH is associated with high mortality rates, a study among 101 confirmed cases in Guatemala found a crude mortality rate of 44% with a median survival time of 19 days (AJTMH 2017,97:42); a Peruvian case series from a single center found that 59% (16) of 27 HIV-infected patients with histoplasmosis had PDH, with a mortality rate of 22% (Rev Chilena Infectol 2017;34:365-9). Co-infections are common. Among 45 patients in Colombia, 23 had other infections, 70% had TB and 13% had PCP or cryptococcosis (Med Mycol Case Rep 2018;19:45) USA treatment guidelines (Clin Infect Dis 2007;45:807) recommend induction therapy with liposomal amphotericin B (or amphotericin B deoxycholate in persons with low risk for nephrotoxicity) for 1-2 weeks followed by itraconazole for at least 1 year, with dosing guided by measurement of serum drug levels. Suppressive therapy with itraconazole is stopped if patients have received one year of itraconazole therapy, have negative blood cultures, low levels of urinary antigen (<2ng/ml), a CD4 cell count >150 cells/mm3, and patients are on HAART. Initiation of HAART should not be delayed; IRIS is rare and usually not severe. Our patient was started empirically on anti TB treatment with standard 4-drug therapy and is currently receiving amphotericin deoxycholate. He will be started on ART within 2 weeks of induction therapy with amphotericin B. |