$3.3 million R01 grant funds research on telehealth cardio program for wheelchair user
 Jereme D. Wilroy, Ph.D., assistant professor for the University of Alabama at Birmingham Department of Physical Medicine and Rehabilitation, was awarded a $3.3 million R01 grant from the National Institutes of Health for his study, “Examining the effects of live telehealth exercise training on cardiometabolic outcomes in wheelchair users."
Jereme D. Wilroy, Ph.D., assistant professor for the University of Alabama at Birmingham Department of Physical Medicine and Rehabilitation, was awarded a $3.3 million R01 grant from the National Institutes of Health for his study, “Examining the effects of live telehealth exercise training on cardiometabolic outcomes in wheelchair users."
UAB offers one of the only multidisciplinary adult spina bifida clinics in the southeastern United States
 Spina bifida is the most common permanently disabling birth defect that is associated with life. Each year approximately 1,400 babies born in the United States have spina bifida, according to the U.S. Centers for Disease Control and Prevention. Spina bifida, usually apparent at birth, is a type of neural tube defect in which the neural tube does not completely close during development in the womb resulting in damage to the spinal cord and nerves.
Spina bifida is the most common permanently disabling birth defect that is associated with life. Each year approximately 1,400 babies born in the United States have spina bifida, according to the U.S. Centers for Disease Control and Prevention. Spina bifida, usually apparent at birth, is a type of neural tube defect in which the neural tube does not completely close during development in the womb resulting in damage to the spinal cord and nerves.
UAB PM&R Faculty Receive Promotions in 2023
 The UAB Department of Physical Medicine and Rehabilitation is pleased to announce the promotion of three faculty members, including two researchers and one neuropsychologist effective Oct. 1, 2023.
The UAB Department of Physical Medicine and Rehabilitation is pleased to announce the promotion of three faculty members, including two researchers and one neuropsychologist effective Oct. 1, 2023.
Dr. Cowan’s World Health Organization Global Wheelchair Service Guidelines Launched
 Rachel Cowan, Ph.D., associate professor at the University of Alabama at Birmingham’s Department of Physical Medicine & Rehabilitation and program co-director for UAB’s Spinal Cord Injury Model System, co-chaired the World Health Organization (WHO) Global Wheelchair Service Guidelines Develop Group (GDG) and co-authored the Wheelchair Service Guidelines alongside Kylie Shae and Sarah Sheldon. The Guidelines were official launched at the April 2023 meeting of the International Society for Prosthetics and Orthotics in Guadalajara, Mexico.
Rachel Cowan, Ph.D., associate professor at the University of Alabama at Birmingham’s Department of Physical Medicine & Rehabilitation and program co-director for UAB’s Spinal Cord Injury Model System, co-chaired the World Health Organization (WHO) Global Wheelchair Service Guidelines Develop Group (GDG) and co-authored the Wheelchair Service Guidelines alongside Kylie Shae and Sarah Sheldon. The Guidelines were official launched at the April 2023 meeting of the International Society for Prosthetics and Orthotics in Guadalajara, Mexico.
UAB residency program shows national reputation in top 25
 UAB Marnix E. Heersink School of MedicineDepartment of Physical Medicine and Rehabilitation's residency program ranks in the top 25 by reputation in Doximity’s Residency Navigator.
UAB Marnix E. Heersink School of MedicineDepartment of Physical Medicine and Rehabilitation's residency program ranks in the top 25 by reputation in Doximity’s Residency Navigator.
PM&R Research Summary: Caregiver resilience six months after traumatic brain injury
 The UAB Traumatic Brain Injury Model System (UAB-TBIMS) conducts independent and collaborative research projects. The UABTBIMS was part of a recent collaborative research study on the resilience of caregivers at six months following traumatic brain injury (TBI). The Virginia Commonwealth Traumatic Brain Injury Model System led the multi-center study, and other participating centers included Mayo Clinic Traumatic Brain Injury Model System, Indiana Traumatic Brain Injury Model System, Rocky Mountain Regional Brain Injury System, and the Northern New Jersey Traumatic Brain Injury System.
The UAB Traumatic Brain Injury Model System (UAB-TBIMS) conducts independent and collaborative research projects. The UABTBIMS was part of a recent collaborative research study on the resilience of caregivers at six months following traumatic brain injury (TBI). The Virginia Commonwealth Traumatic Brain Injury Model System led the multi-center study, and other participating centers included Mayo Clinic Traumatic Brain Injury Model System, Indiana Traumatic Brain Injury Model System, Rocky Mountain Regional Brain Injury System, and the Northern New Jersey Traumatic Brain Injury System.
UAB PM&R joins Limb Loss & Preservation Registry
 The University of Alabama at Birmingham’sDepartment of Physical Medicine and Rehabilitation, a prosthetics and orthotics patient care provider, has joined the Limb Loss & Preservation Registry (LLPR).
The University of Alabama at Birmingham’sDepartment of Physical Medicine and Rehabilitation, a prosthetics and orthotics patient care provider, has joined the Limb Loss & Preservation Registry (LLPR).
PM&R Research Publication Quick Review: Effects of a Low-Carbohydrate, High-Protein Diet on Gut Microbiome Composition
 Past research suggests that an imbalance of gut bacteria develops after spinal cord injury (SCI). This imbalance can lead to cardiometabolic diseases like obesity, diabetes, insulin resistance, and non-alcoholic fatty liver disease.
Past research suggests that an imbalance of gut bacteria develops after spinal cord injury (SCI). This imbalance can lead to cardiometabolic diseases like obesity, diabetes, insulin resistance, and non-alcoholic fatty liver disease.
Brewer selected for UAB Medicine Institute for Leadership
 Good leadership is key to any organization, and UAB is no exception. UAB’s Department of Physical Medicine & Rehabilitation is proud to announce that Administrative Director Tracy Brewer joins the FALL 2023 cohort of the UAB Medicine Institute for Leadership.
Good leadership is key to any organization, and UAB is no exception. UAB’s Department of Physical Medicine & Rehabilitation is proud to announce that Administrative Director Tracy Brewer joins the FALL 2023 cohort of the UAB Medicine Institute for Leadership.
McShan appointed to the American Heart Association 2023-2024 Southeast Board of Directors
 Dr. Andre’ McShan, Assistant Professor in the Department of Physical Medicine and Rehabilitation, and Medical Director for the Occupational Medicine program at The Workplace-UAB Highlands, was selected to serve on the American Heart Association 2023-2024 Southeast Board of Directors.
Dr. Andre’ McShan, Assistant Professor in the Department of Physical Medicine and Rehabilitation, and Medical Director for the Occupational Medicine program at The Workplace-UAB Highlands, was selected to serve on the American Heart Association 2023-2024 Southeast Board of Directors.
McShan is a longtime advocate for the American Heart Association. He has served on the board at the local level including his role as past president. In this new appointment, McShan will serve a 3-year term for the Southeast regional board of directors as well as a member of the Health Equity and Workplace Health Steering Committees.
“Heart disease remains the number one cause of death in the United States and disproportionately effects minority communities,” said McShan. “Like many others, I’ve experienced personal loss due to heart disease and stroke. I’m honored to be a part of this organization, and I’m excited to use my expertise to expand the efforts of the American Heart Association.”
The board will meet quarterly and rotate to different host cities around the southeast. Their current regional initiatives include topics such as addressing teen vaping, helping to decrease food insecurity, and reinforcing blood pressure guidelines.
The American Heart Association is a nonprofit organization in the United States that funds cardiovascular medical research, educates consumers on healthy living and fosters appropriate cardiac care in in an effort to reduce disability and deaths caused by cardiovascular disease and stroke.
Biney and Wen named recipients of CEDHARS pilot program
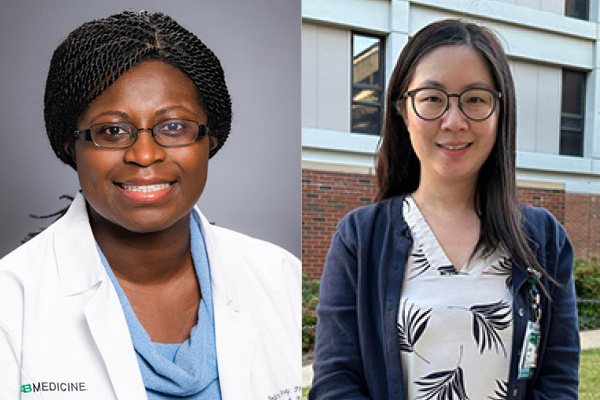 The Center for Engagement in Disability Health and Rehabilitation Sciences (CEDHARS) selected Fedora Biney, Ph.D. and Huacong Wen, Ph.D. as recipients of its spring 2023 pilot grant funding opportunity, “Secondary Data Analysis to Advance Health or Rehabilitation Outcomes Research in People with Disabilities.”
The Center for Engagement in Disability Health and Rehabilitation Sciences (CEDHARS) selected Fedora Biney, Ph.D. and Huacong Wen, Ph.D. as recipients of its spring 2023 pilot grant funding opportunity, “Secondary Data Analysis to Advance Health or Rehabilitation Outcomes Research in People with Disabilities.”
PM&R Welcomes PGY1 and PGY2 Residents
 The University of Alabama at BirminghamDepartment of Physical Medicine and Rehabilitation Residency Training Program welcomed a group of eight new residents in July.
The University of Alabama at BirminghamDepartment of Physical Medicine and Rehabilitation Residency Training Program welcomed a group of eight new residents in July.
Chen Promoted to PM&R Vice Chair of Research
 Professor Yuying Chen, M.D., Ph.D. has been promoted to Vice Chair of Research for the Department of Physical Medicine and Rehabilitation (PM&R) in the UAB Marnix E. Heersink School of Medicine (HSOM). Chen served as Research Director prior to her promotion.
Professor Yuying Chen, M.D., Ph.D. has been promoted to Vice Chair of Research for the Department of Physical Medicine and Rehabilitation (PM&R) in the UAB Marnix E. Heersink School of Medicine (HSOM). Chen served as Research Director prior to her promotion.
Dr. Chen joined the department of PM&R faculty in 2000 and has served as Project Director of the National Spinal Cord Injury Statistical Center since 2005. She has gained international recognition for her research involving epidemiology, mortality, and secondary conditions after spinal cord injury (SCI), including obesity, racial health disparities, and social determinants of health. Chen’s most recent honors include being selected to serve on the American Spinal Injury Association Board of Directors, awarded The American Congress of Rehabilitation Medicine’s (ACRM) SCI Interdisciplinary Special Interest Group Margaret Nosek Award, selected for the UAB Healthcare Leadership Academy Class of 2023, and recognized by The Archives of Physical Medicine and Rehabilitation with the Most Cited Original Research Article Award.
“It is my privilege and honor to promote Dr. Chen to the Vice Chair of Research role. She is a passionate researcher who, through her work, has greatly advanced the worldwide standard of care for those living with spinal cord injury,” states Vu Nguyen, M.D., chair of the Department. We are very fortunate to have had her leadership over the years. It is my hope that we can capture her energy and brilliance to elevate the level of research in the department and at UAB. It’s a great day for UAB PM&R research,” exclaims Nguyen.”
Dr. Chen is a board-certified physiatrist from Taiwan and epidemiologist with extensive training and experience in database management, research methodology, and statistical analysis. She has led a number of studies and published more than 94 manuscripts in peer-reviewed journals, many of which involved the use of the National SCI Database.
“I look forward to this new chapter of my research career, leading a team of remarkable researchers to expand the Department’s research portfolio and advance rehabilitation science,” said Dr. Chen.
Dr. Chen is the Co-Director for the UAB Center for Engagement in Disability Health and Rehabilitation Sciences. She also serves on the Heersink School of Medicine Faculty Council and Committee on Responsible Research Practices as well as PM&R’s Promotion and Tenure, Finance, Journal Club, and Grand Rounds Committees.
Crash Risk Following Return to Driving After Moderate-to-Severe TBI: A TBI Model Systems Study
 The UAB Traumatic Brain Injury Model System (UAB-TBIMS) led a collaborative research study on crash risk following return to driving after moderate-to-severe TBI. Collaborative centers included the Virginia Traumatic Brain Injury Model System, Mayo Clinic Traumatic Brain Injury Model System, University of Washington Traumatic Brain Injury Model System, Moss Traumatic Brain Injury Model System, Rocky Mountain Regional Brain Injury System, Southeastern Michigan Traumatic Brain Injury System, and JFK Johnson Rehabilitation Institute.
The UAB Traumatic Brain Injury Model System (UAB-TBIMS) led a collaborative research study on crash risk following return to driving after moderate-to-severe TBI. Collaborative centers included the Virginia Traumatic Brain Injury Model System, Mayo Clinic Traumatic Brain Injury Model System, University of Washington Traumatic Brain Injury Model System, Moss Traumatic Brain Injury Model System, Rocky Mountain Regional Brain Injury System, Southeastern Michigan Traumatic Brain Injury System, and JFK Johnson Rehabilitation Institute.
All eight TBI Model Systems sites conducted a phone survey to interview a total of 438 adults with TBI who returned to driving. The aim was to look at the number of motor vehicle crashes and risk factors of crashes for people after moderate-to-severe TBI. Participants were asked about their confidence in driving, driving ability, and history of crashes. Those interviewed were of different ages, time since injury, injury severity, sex, employment status, marital status, education levels, location, family income, and seizure history in the year prior to survey.
The study found that the people with TBI who participated in this study were 1.5 to 2.5 times more likely to be in crashes over a one-year timeframe when compared to the general population. Although the crash risk is higher following TBI than the general population, the results do not justify restricting people from driving after TBI as most people reported not having any crashes after their injury. However, there remains a need to identify and address factors that increase crash risk after TBI.
This study was funded by the National Institute on Disability, Independent Living, and Rehabilitation Research and published in the Journal of Head Trauma Rehabilitation .
2023 UAB PM&R Resident Graduation
 Congratulations to our newest class of graduating residents on their completion of the UAB Heersink School of Medicine Department of Physical Medicine and Rehabilitation residency program. Our 2023 graduates include Lendrum Morrow, M.D., Jacob Schultz, M.D., Ashley Steffens, M.D., and Brea Willeford, D.O.
Congratulations to our newest class of graduating residents on their completion of the UAB Heersink School of Medicine Department of Physical Medicine and Rehabilitation residency program. Our 2023 graduates include Lendrum Morrow, M.D., Jacob Schultz, M.D., Ashley Steffens, M.D., and Brea Willeford, D.O.
The department is excited to watch each graduate create their own path for success in medicine. Lendrum Morrow, M.D. is doing an Interventional Spine and MSK Fellowship at OrthoAlabama Spine and Sport in Birmingham, AL. Jacob Schultz, M.D. will continue as an assistant professor and attending physician at Frazier Rehabilitation Institute Dept. of Neurosurgery in Louisville, KY. Ashley Steffens, M.D. is relocating to Mobile, AL to be an attending inpatient physician at JL Bedsole Rotary Rehabilitation Hospital. Brea Willeford, D.O. will remain at UAB to do a Pain Medicine Fellowship with UAB Department of Anesthesia.
The graduation ceremony took place on July 15, 2023 at The Fennec in downtown Birmingham. In addition to celebrating our graduates, awards were given to staff and residents who have gone above and beyond in PM&R.
Resident Anchor Award - This annual award is given to a non-faculty member who goes above and beyond their regular duties to best support the residents. This person exemplifies a high level of dedication to the residents, as well as their normal role and responsibilities. This award is voted on by the residents and given annually to a non-faculty member that the residents feel best exemplifies the spirit of this award in all that they do in their daily role.
Recipient: Savannah Tinsley, PM&R Residency Program Education Coordinator
Laura B. Kezar Award for Dedication and Commitment to the Residency Program - This annual award is named for Dr. Laura B. Kezar who served as a valued member of the PM&R Faculty as well as the PM&R Residency Program Director from 1996 to 2007, and the Assistant Program Director from 2007 to 2014. Throughout her tenure with the department, Dr. Kezar has always made the PM&R Residency Program and education for all a top priority. Her dedication and commitment was noted by every residency class. She served not only as a teacher and educator, but also mentor to a countless number of residents over the years. This award is voted on by the residents and given annually to a faculty member that the residents feel best exemplifies the spirit of this award in all that they do in their daily practice.
Recipient: Berdale Colorado, D.O.
Samuel L. Stover Excellence in Teaching Award - This annual award is named for Dr. Samuel L. Stover who served as a valued member of the PM&R Faculty as well as Chair of the Department of PM&R from 1976 to 1994. Dr. Stover was known as a lifelong learner and throughout his career placed great emphasis on education. He felt the education of our residents should be a top priority for the department and instilled this expectation in all of our faculty members through the years. This award is voted on by the residents and given annually to a faculty member that the residents feel best exemplifies the spirit of this award.
Recipient: Vu Nguyen, M.D.
C.T. Huang Award - This award is intended to go to the resident that the department feels best exemplifies high clinical excellence during their training.
Recipient: Ashley Steffens, MD
Outstanding PGY2 Award - This award is given to a deserving second year resident who consistently displays excellence in professionalism, patient care, accountability, integrity and leadership during his or her initial year of training at Spain Rehabilitation Center.
Recipient: Cynthia Francis, M.D.
Matthew T. Smith Humanism in Medicine Award - This award is given to a PM&R Faculty Member and a PM&R Resident who has excelled in service to others during his/her tenure with the Department of PM&R. It is intended to honor those who exemplify Dr. Smith’s qualities of compassionate caring, support for others, teamwork, involvement in community and UAB activities and upholding the highest standards of practice.
Resident Recipient: Brea Willeford, D.O.
Faculty Recipient: Cassandra Renfro, D.O.
Resident Research Award - This a newly developed award collaborated by the Research department and Residency Education Office. This award is given to a resident who has demonstrated exemplary overall research efforts. Recipient: Daniel McBride, M.D. PGY 4 Research Presentation Award – This a newly developed award collaborated by the Research department and Residency Education Office. This award is voted by attendees of Grand Rounds following the PGY4 poster presentations and is given to the senior resident with the most outstanding research poster.
Recipient: Lendrum Morrow, M.D.
Highest SAE Score Award Recipients
PGY2 – Darien McNeill, M.D.
PGY3 – Sarah Lopes, D.O.
PGY4 – Brea Willeford, D.O.
Latorre and Cowan elected to represent Heersink School of Medicine on the UAB Faculty Senate
 Johan Latorre, M.D. and Rachel Cowan, Ph.D., both faculty members in the Department of Physical Medicine and Rehabilitation, have been elected to represent Heersink School of Medicine on the 2023-2025 UAB Faculty Senate.
Johan Latorre, M.D. and Rachel Cowan, Ph.D., both faculty members in the Department of Physical Medicine and Rehabilitation, have been elected to represent Heersink School of Medicine on the 2023-2025 UAB Faculty Senate.
The Faculty Senate represents UAB’s faculty in matters of shared governance. The Senate is made up of faculty representatives from all of UAB’s academic units, as well as four officers elected at large by the faculty. Through participation in various councils and committees, the senators will convey the faculty’s views and concerns in matters that affect our University.
“I have been a part of multiple large organizations within institutions such as the Resident Physician Union at the University of Michigan that helped improve the lives of the residents. Now as faculty at UAB, I want to do the same. Being a Senator allows me to have a say in the direction UAB takes and not just the health system/medical school community but the campus as a whole,” Dr. Latorre said.
The incoming Chair of the Faculty Senate, Karen Cropsey, will assign every Senate member to serve as a member of a Faculty Senate Standing Committee. Some senate members may also be asked to serve on University-wide Committees. This two-year service term begins September 1, 2023, and ends August 31, 2025.
“I’m honored to serve as a faculty senator for UAB. It gives me the opportunity to learn more about university operations at a higher level outside my area of research. I’m glad I can be a voice for the concerns of researchers not heard outside Heersink School of Medicine.” Dr. Cowan stated.
UAB PM&R set to launch its latest research study into the importance of microbiome on health and function after spinal cord injury

Simply put, microbiome is all of the microscopic microbes that live on and in our bodies. This includes bacteria, fungi, viruses, and their genes.
The UAB Department of Physical Medicine and Rehabilitation has been at the forefront of the emerging research into the importance of microbiome on health and function after spinal cord injury (SCI). With its latest research, UAB aims to look specifically into the impact of gut microbiome on metabolic and bowel function during the first year after SCI.
“There’s typically slower intestinal movement of waste after SCI that leads to leakage of bile and harmful bacteria into the bloodstream,” says Jereme Wilroy, Ph.D., principal investigator and assistant professor in the Department. “Harmful bacteria in the blood can damage the body’s organs and lead to metabolic disorders and associated complications like obesity, insulin resistance and type 2 diabetes, all conditions that people with chronic SCI are at an increased for developing.”
For the study, patients will be enrolled in the first few weeks after injury and followed for a year. During that time, periodic blood and stool samples will be collected along with surveys of their bowel function. Samples will be analyzed for microbiome changes. Finding changes may lead to the development of an inexpensive, non-invasive diet- or supplement-based treatment option for improving the health and quality of life for persons with SCI.
This study is the site-specific research project of the UAB Spinal Cord Injury Model System.
UAB Spina Bifida Program shines on a global stage
 At the largest World Congress on Spina Bifida Research and Care (SBWC) in event history, representatives from the University of Alabama at Birmingham and Children’s of Alabama made up 17% of the total platform presentations, with 23 oral and 13 poster presentations.
At the largest World Congress on Spina Bifida Research and Care (SBWC) in event history, representatives from the University of Alabama at Birmingham and Children’s of Alabama made up 17% of the total platform presentations, with 23 oral and 13 poster presentations.
Colorado selected for national expert panel on orthobiologics
 Dale Colorado, D.O., M.P.H. was selected to serve on the American Academy of Physical Medicine and Rehabilitation (AAPM&R) Technical Expert Panel for orthobiologic management of osteoarthritis of the knee. The panel will develop and author a clinical practice guidance statement to advance knowledge and promote standards of care and best practices based on the best available evidence.
Dale Colorado, D.O., M.P.H. was selected to serve on the American Academy of Physical Medicine and Rehabilitation (AAPM&R) Technical Expert Panel for orthobiologic management of osteoarthritis of the knee. The panel will develop and author a clinical practice guidance statement to advance knowledge and promote standards of care and best practices based on the best available evidence.
"While the research on orthobiologics is ever-expanding, there is still a lot that we don't know. I am excited to help guide and inform healthcare providers regarding the use of orthobiologics for knee osteoarthritis," stated Colorado.
Dr. Colorado has been using orthobiologics in his clinical practice for approximately 10 years. He was Founder and Medical Director of the Orthopedic Regenerative Medicine Program in the Department of Orthopedic Surgery at Washington University in St. Louis. He has given numerous lectures/presentations on regenerative medicine.
Dr. Colorado is Associate Professor and Vice Chair of Education in the Department of Physical Medicine and Rehabilitation (PM&R) at the University of Alabama at Birmingham (UAB). He serves as PM&R Residency Program Director and Medical Director of Sports and Musculoskeletal Medicine. Dr. Colorado is also a team physician for UAB Athletics and a part of the UAB Sports & Exercise Medicine program.
PM&R researchers using simulator to assess return to driving after traumatic brain injury
 Driving is one of the hallmarks of a person’s independence, but people who experience moderate-to-severe traumatic brain injury (TBI) often have physical and cognitive deficits that limit their ability to return to driving. Such deficits might include response speed, maintenance of lane position, vehicle speed and stopping, response to distraction, attention to the roadway, identification of road hazards, and crash risk.
Driving is one of the hallmarks of a person’s independence, but people who experience moderate-to-severe traumatic brain injury (TBI) often have physical and cognitive deficits that limit their ability to return to driving. Such deficits might include response speed, maintenance of lane position, vehicle speed and stopping, response to distraction, attention to the roadway, identification of road hazards, and crash risk.
A new study launched by researchers at the Department of Physical Medicine and Rehabilitation aims to look at the value of using a driving simulator to predict on-road driving performance after TBI.
“We know that most people who return to driving after a TBI do so safely, and it has an enormously positive impact on mental wellbeing, sense of independence, community reintegration along with health and function,” says Instructor Jenny Marwitz, project co-director and the department’s Director of TBI Research. “And we know that the most common driving assessments are typically not designed to identify specific safety concerns that a person with TBI might have. We want to see if a driving simulator built to identify deficits is a good option. Then, we can work with therapists to develop strategies to target deficits.”
The driving simulator chosen for the study is a compact and economical option for most rehabilitation centers to implement into clinical practice. It offers a series of driving scenarios designed as distinct modules to simulate a specific driving task, environment, or situation that increases in visual and strategic complexity of the environment and strategic control. Participants have a first-person point of view of the interior rearview mirror and dashboard, along with full left to right exterior field of view, with side mirrors.
“Another goal is the development of guidelines for clinicians to help people with TBI return to driving, and do it safely,” adds Marwitz. “We think the compact simulator can be a more accessible and affordable way to make that happen.”
This study is the site-specific research project of the UAB Traumatic Brain Injury Model System.