 |
Gorgas Case 2022-05 |
 |
|
The following patient was seen in the dermatology clinic at Cayetano Heredia Hospital. We would like to thank Dr. Francisco Bravo and the staff at the dermatology clinic for their assistance with this case.  History: A 21-year-old male presented with a 4-year history starting with a cut on his right sole while swimming in a river. One month after the cut, he noticed a skin-colored papule in the area of the lesion; more papules with the same characteristics appeared over the following months, with swelling and pain in the affected limb. 3 years before presentation, he was diagnosed with an unspecified mycosis and received treatment with topical econazole, without improvement. 1 year before presentation, the lesions extended to the dorsum of the right foot, and 5 months before admission he sought attention at a peripheral hospital and was referred to our institution for further study. Epidemiology: Born in Caraz, in the central highlands of Peru, and lives in Huaral, in the highlands of Lima. He is not currently working. No TB contacts, no ill family members. Physical Examination: T 36º, BP 100/60 mmHg, HR 80 bpm, RR 20 rpm, Sat 99% (FiO2 0.21). Patient appeared well, but had moderate pain in the left foot and had difficulty stepping with that foot. Verrucous lesion in dorsum and sole of left foot, with significant localized edema, fistula formation, and white purulent exudate with orange granules [Images A and B]. No regional lymphadenopathy was noted. The rest of the physical exam was unremarkable. Laboratory: Hb: 14.8 g/dl, Hct: 47%; WBC 6870 (bands 0%, segmented 57%, eosinophils 0%), Platelets 192 000; Glucose 87 mg/dL, Creatinine 0.67 mg/dL, BUN 41 mg/dL; AST 24 U/L, ALT 20 U/L; Total protein 7.3 mg/dL, albumin 4.1 mg/dL; HIV 1-2 HTLV-1 and VDRL/RPR were non-reactive. Imaging: Soft tissue ultrasound showed a mass with heterogeneous contents, predominantly hypoechoic, with alternating hyperechoic areas that project onto deeper planes, with little vascularization on Doppler. X-rays showed increased volume and changes in the density of soft tissues, predominantly on the lateral side of the right foot, with no muscular or bone involvement [Image C].
|
|
Diagnosis: Botryomycosis caused by Staphylococcus epidermidis. 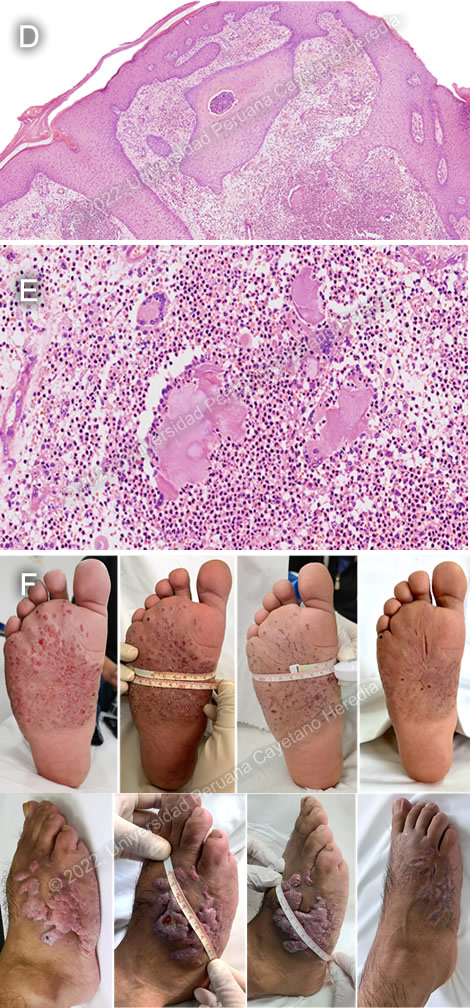
 Discussion: A skin biopsy revealed a pseudoepithelial hyperplasia of the epidermis and many nodular infiltrates in the superficial and deep dermis (red arrow) [Image D]. On higher magnification, the nodules were revealed to include a mix of lymphocytes, neutrophils, histiocytes and giant multinucleated cells, with Splendore-Hoeppli phenomenon (intense eosinophilic reaction between the granules) [Image E]. Ziehl-Neelsen and PAS stains were negative, as were AFB and fungal cultures. Cultures grew Staphylococcus epidermidis, and a diagnosis of botryomycosis due to S. epidermidis was made. Botryomycosis is an uncommon chronic bacterial infection with a global distribution in the tropics and non-tropics that is characterized by a granulomatous inflammatory response to bacterial pathogens [Clin Dermatol. 2012 Jul-Aug;30(4):397-402]. The disease is characterized by the presence of granules containing a central mass of bacteria within an area of pus. In the tropics, clinically and histologically, botryomycosis can mimic both eumycetoma (Madura foot) [see Gorgas Case 2002-04] due to fungal etiologies (black grains) as well as actinomycetoma due to bacteria (Nocardia, Actinomadura [red grains], or Streptomyces [white/yellow grains]). Other differential diagnoses for an infiltrated tumor with granulomatous papules and nodules include pseudomycetoma, localized verruga peruana, saroma, Ledderhose disease, angiolymphoid hyperplasia, and cutaneous sarcoidosis. Up to one-third of cases of botryomycosis present with only deep visceral involvement, usually in debilitated patients. Until Staphylococcus aureus was cultured from lesions in 1919, botryomycosis was believed to be fungal in nature, hence the name. The infection is uncommon but no specific incidence data is available. The literature consists of about 200 case reports and no large case series, but we have seen at least 5 cases in recent years suggesting it is not as rare as the numbers in the published literature. Staphylococcus aureus causes the majority of infections, followed by Pseudomonas aeruginosa and then a long list of other bacteria. Botryomycosis due to S. epidermidis has been previously reported, accounting for as many as 2.4% of cases [Int. J. Dermatol. 1996 June;35(6):382]. Pathogenesis is not clear but limited animal work suggests that it is related to bacterial strains, inoculum of bacteria, and perhaps host immune response. Frequent findings of intracellular bacteria suggest a host immune defect. Most of the individual case reports have been in individuals with impaired T-cell immunity of one sort or another, including HIV infection as well as those with diabetes as well as liver disease, but again there are no systematic incidence studies. One of the cases we have seen was HTLV-1 positive. Visceral cases have been reported. A diagnosis can be established through identification of nonfilamentous bacteria in gram stains of crushed granules or biopsies, and supported by isolation of bacterial pathogens in culture and typical histopathologic features (central focus of necrosis with chronic inflammatory reaction with Splendore-Hoeppli phenomenon). Our patient was started on oral antibiotics (clindamycin 300mg q8h PO and ciprofloxacin 500mg q12h PO, on the basis of drug sensitivities in culture) and bimonthly intralesional injections of lincomycin, with marked improvement in symptoms and near resolution of the skin lesions after two years [Image F]. |