The first, "Targeted Sequencing of Plasmacytoid Urothelial Carcinoma Reveals Frequent TERT Promoter Mutations," was published in the March 2019 issue, Volume 85.
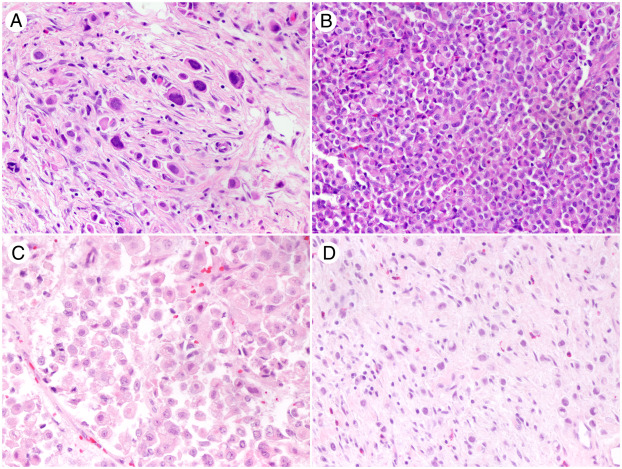
The article's summary follows: "Activating mutations in the promoter of the telomerase reverse transcriptase (TERT) gene are the most common genetic alterations in urothelial carcinoma (UC) of the bladder and upper urinary tract. Although the cadherin 1 (CDH1) gene is commonly mutated in the clinically aggressive plasmacytoid variant of urothelial carcinoma (PUC), little is known about their TERT promoter mutation status. A retrospective search of our archives for PUC and UC with plasmacytoid and/or signet ring cellfeatures (2007-2014) was performed. Ten specimens from 10 patients had archived material available for DNA analysis and were included in the study. Intratumoral areas of nonplasmacytoid histology were also evaluated when present. Samples were analyzed for TERT promoter mutations with Safe-SeqS, a sequencing error-reduction technology, and sequenced using a targeted panel of the 10 most commonly mutated genes in bladder cancer on the Illumina MiSeq platform. TERT promoter mutations were detected in specimens with pure and focal plasmacytoid features (6/10). Similar to conventional UC, the predominant mutation identified was g.1295228C>T. In heterogeneous tumors with focal variant histology, concordant mutations were found in plasmacytoid and corresponding conventional, glandular, or sarcomatoid areas. Co-occurring mutations in tumor protein p53 (TP53, 2 cases) and kirsten rat sarcoma (KRAS) viral proto-oncogene (1 case) were also detected. TERT promoter mutations are frequently present in PUC, which provides further evidence that TERT promoter mutations are common events in bladder cancer, regardless of histologic subtype, and supports their inclusion in any liquid biopsy assay for bladder cancer."
Maria del Carmen Rodriguez Pena, M.D., postdoctoral fellow, UAB Pathology, is also an author on the article.
The second and most recent is entitled, "Tumor Immune Microenvironment in Non-Muscle-Invasive Urothelial Carcinoma of the Bladder," will be published in the forthcoming July 2019 issue of Human Pathology, Volume 89.
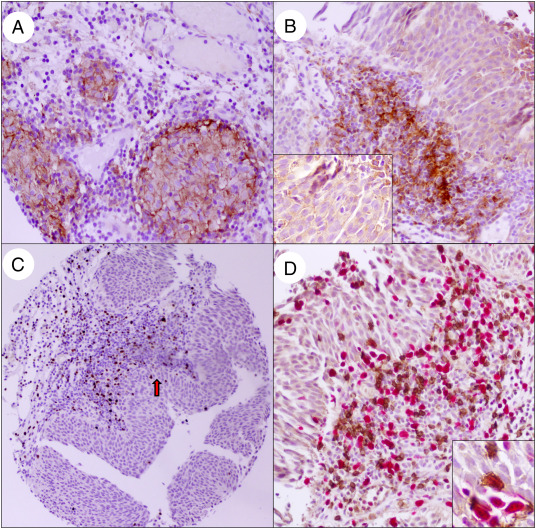
The summary for the article follows: "Immunotherapy has gained significance in a variety of tumor types including advanced urothelial carcinoma. Noninvasive urothelial lesions have been treated with intravesical Bacillus-Calmette-Guerin (BCG) for decades. Given treatment failure in a subset of these tumors, ongoing clinical trials investigating the role of checkpoint inhibitors are actively pursued in this group of patients. The present study aims to delineate PD-L1, CD8, and FOXP3 expression in tumor microenvironment in non–muscle-invasive urothelial carcinoma samples obtained via sequential biopsies and to assess its potential role in predicting disease outcome. Cases with >1% and> 5% PD-L1 expression in tumor cells showed lower relative risk (RR) to recur at any subsequent biopsy compared with those with lower PD-L1 expression (RRs, 0.83 [P = .009] and 0.81 [P = .03], respectively). Cases with higher expression of FOXP3 in peritumoral lymphocytes were at lower risk for tumor grade progression at any biopsy (RR, 0.2; P = .02). Tumors with FOXP3/CD8 expression ratio of >1 in intratumoral lymphocytes had lower risk of grade progression (RR, 0.28; P = .04). Although higher number of FOXP3-, CD8-, and PD-L1–positive lymphocytes were encountered after BCG treatment, the findings did not reach statistical significance. In patients without BCG treatment, PD-L1 expression in tumor cells and peritumoral lymphocytes varied across serial biopsies, suggesting the need for additional approaches to assess eligibility for immunotherapy in non–muscle-invasive urothelial carcinoma patients."
del Carmen Rodriguez Pena, M.D., and Marie-Lisa Eich, M.D., postdoctoral fellow, are both authors on the article.
All three authors also collaborated on an article published in Modern Pathology in April, "Incidence and Distribution of UroSEEK Gene Panel in a Multi-Institutional Cohort of Bladder Urothelial Carcinoma."
The summary is, "Noninvasive approaches for early detection of bladder cancer are actively being investigated. We recently developed a urine- based molecular assay for the detection and surveillance of bladder neoplasms (UroSEEK). UroSEEK is designed to detect alterations in 11 genes that include most common genetic alterations in bladder cancer. In this study, we analyzed 527 cases, including 373 noninvasive and 154 invasive urothelial carcinomas of bladder from transurethral resections or cystectomies performed at four institutions (1991–2016). Two different mutational analysis assays of a representative tumor area were performed: first, a singleplex PCR assay for evaluation of the TERTpromoter region (TERTSeqS) and second, a multiplex PCR assay using primers designed to amplify regions of interest of 10 (FGFR3, PIK3CA, TP53, HRAS, KRAS, ERBB2, CDKN2A, MET, MLL, and VHL) genes (UroSeqS). Overall, 92% of all bladder tumors were positive for at least one genetic alteration in the UroSEEK panel. We found TERT promoter mutations in 77% of low-grade noninvasive papillary carcinomas, with a relatively lower incidence of 65% in high-grade noninvasive papillary carcinomas and carcinomas in situ; p = 0.017. Seventy-two percent of pT1 and 63% of muscle-invasive bladder tumors harbored TERTpromoter mutations with g.1295228C>T alteration being the most common in all groups. FGFR3 and PIK3CA mutations were more frequent in low-grade noninvasive papillary carcinomas compared with high-grade noninvasive papillary carcinomas and carcinomas in situ (p < 0.0001), while the opposite was true for TP53 (p < 0.0001). Significantly higher rates of TP53 and CDKN2A mutation rates (p = 0.005 and 0.035, respectively) were encountered in muscle-invasive bladder tumors compared with those of pT1 stage. The overwhelming majority of all investigated tumors showed at least one mutation among UroSEEK assay genes, confirming the comprehensive coverage of the panel and supporting its potential utility as a noninvasive urine-based assay."