| 2011 Case #7 |  |
|
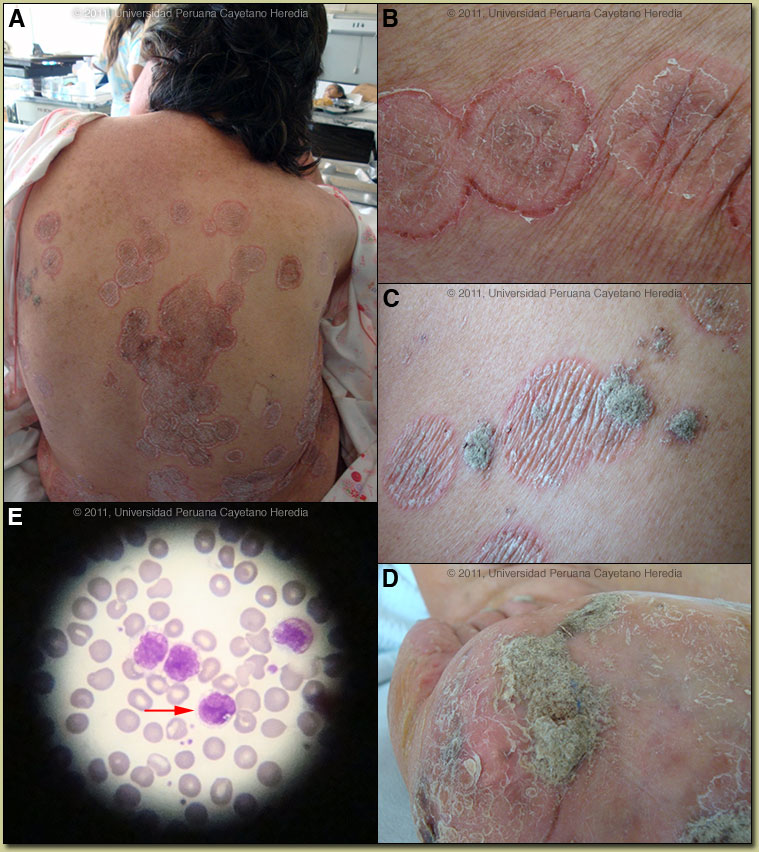
| Diagnosis: HTLV-1 infection with 3 separate cutaneous complications: Adult T-cell leukemia/lymphoma (ATLL), Tinea corporis, and crusted (Norwegian) scabies. |
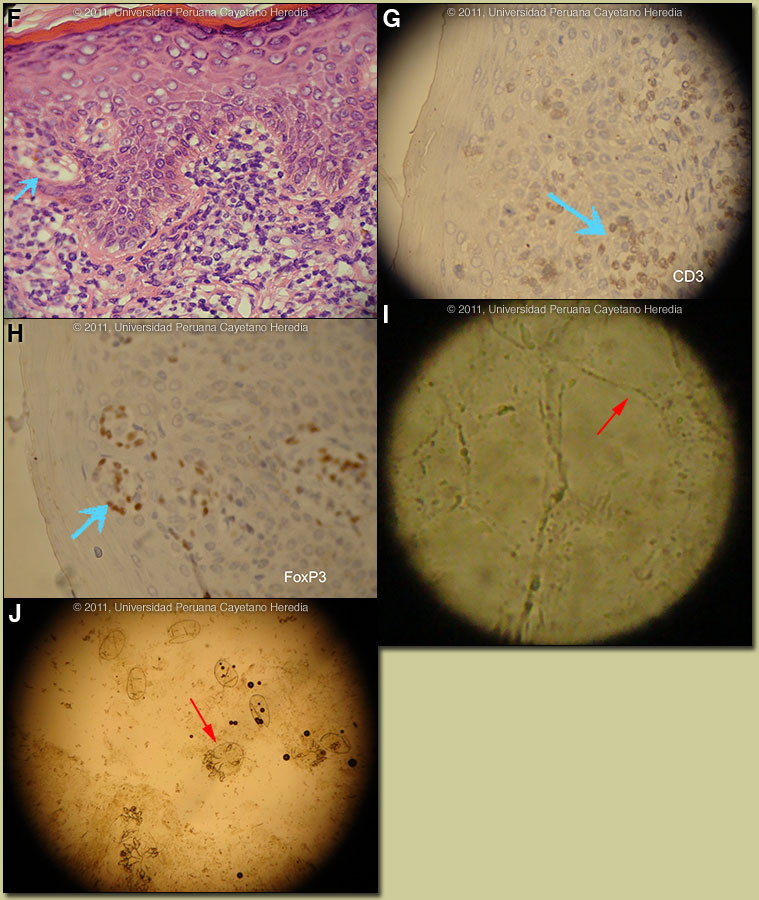 Discussion: Positive western blot for HTLV-1. HIV negative. A skin biopsy from the annular lesions, which appear consistent with a tinea infection, demonstrated marked exocytosis, and the presence of atypical lymphocytes in the epidermis [Image F]. The lymphocytes were hyperchromatic, and they were also present along the dermo-epidermal junction, as well as in the papillary dermis. Those changes by themselves were compatible with cutaneous involvement by ATLL. Surprisingly, the PAS staining showed the presence of hyphae in the stratum corneum of the same biopsy. This latter finding confirmed two diagnoses in one biopsy: ATLL and concomitant tinea. Immunostaining for CD3 confirms the T-cell origin and the presence of FoxP3, a marker of T-reg cells, demonstrates cells that are implicated in the pathogenesis of many diseases associated with HTLV-1 [Images G, H]. The histological diagnosis is a T cell lymphoma, but in the context of an HTLV-1 positive patient with clinical lesions not typical of Mycosis fungoides, the diagnosis is certainly ATLL. In an ideal situation, HTLV-1 proviral integration should be demonstrated in the atypical lymphocytes and a sophisticated panel of CD surface markers should be demonstrated on the surface. Scrapings from the annular lesions showed abundant hyphae [Image I]. Profuse Sarcoptes scabei were seen by microscopy from skin scrapings over all the crusty areas [Image J]. Discussion: Positive western blot for HTLV-1. HIV negative. A skin biopsy from the annular lesions, which appear consistent with a tinea infection, demonstrated marked exocytosis, and the presence of atypical lymphocytes in the epidermis [Image F]. The lymphocytes were hyperchromatic, and they were also present along the dermo-epidermal junction, as well as in the papillary dermis. Those changes by themselves were compatible with cutaneous involvement by ATLL. Surprisingly, the PAS staining showed the presence of hyphae in the stratum corneum of the same biopsy. This latter finding confirmed two diagnoses in one biopsy: ATLL and concomitant tinea. Immunostaining for CD3 confirms the T-cell origin and the presence of FoxP3, a marker of T-reg cells, demonstrates cells that are implicated in the pathogenesis of many diseases associated with HTLV-1 [Images G, H]. The histological diagnosis is a T cell lymphoma, but in the context of an HTLV-1 positive patient with clinical lesions not typical of Mycosis fungoides, the diagnosis is certainly ATLL. In an ideal situation, HTLV-1 proviral integration should be demonstrated in the atypical lymphocytes and a sophisticated panel of CD surface markers should be demonstrated on the surface. Scrapings from the annular lesions showed abundant hyphae [Image I]. Profuse Sarcoptes scabei were seen by microscopy from skin scrapings over all the crusty areas [Image J].
On initial clinical presentation, this patient’s lesions over the trunk in a tropical setting provided a broad differential diagnosis. Possibilities include different varieties of tinea, even pityriasis versicolor. Annular lesions always bring to mind the possibility of leprosy; although scaliness to such a degree is not common unless the patient is having a type 1 or type 2 leprosy reaction. Non-infectious processes such as atypical pityriasis rosea or mycosis fungoides have to be included on the basis of clinical appearance alone. Pityriasis rotunda, a condition characterized by multiple round scaly patches over the trunk, with certain similarities to what is seen in this case, has been associated in South African patients with an underlying hepatocellular carcinoma. Adult T-cell leukemia/lymphoma (ATLL) due to HTLV-1 infection is sub-divided into four categories: acute, lymphomatous, chronic, and smoldering [J Clin Oncol. 2009 Jan;27(3):453-9]. The latter two types are considered indolent and may be treated with watchful waiting until disease progression or invasion. This is somewhat analogous to the situation with chronic lymphocytic leukemia (CLL). Patients with the more aggressive forms generally have a poor prognosis (survival <1 year) despite aggressive conventional chemotherapy; many different regimens have provided no measurable benefit. Aggressive forms are associated with hypercalcemia and opportunistic infections. Typical ATLL cells have multi-lobular nuclei with homogeneous and condensed chromatin, small or absent nuclei, and agranular and basophilic cytoplasm. These so-called flower cells were not seen in the biopsy and are generally not seen in the peripheral blood or skin of patients with smoldering disease. Mildly elevated LDH, as in this patient, is often seen in smoldering disease. A number of conditions are associated with HTLV-1 infection; [see Lancet Infect Dis. 2007 Apr;7(4):266-81 for a detailed discussion]. This patient demonstrates at least two major conditions at the same time: crusted (Norwegian) scabies [see also Gorgas Case 2008-08] and adult T-cell leukemia/lymphoma (ATLL) [see Gorgas Case 2009-11]. Others include: strongyloides hyperinfection [see Gorgas Case 2007-04]; tropical spastic paraparesis (TSP), also called HAM (HTLV-1 associated myelopathy) [see Gorgas Case 2002-08], infective dermatitis [see Gorgas Case 2004-07], and autoimmune disease, including uveitis, Sjögrens, arthropathy, polymyositis, tuberculosis, and thyroiditis. Extensive tinea corporis, although non-specific, has also been described as a manifestation of an otherwise undiagnosed HTLV-1 infection. This patient did not have any neurological findings. More than 90% of individuals with HTLV-1 infection remain asymptomatic for life. Worldwide, approximately 0.3-4.0% develop TSP and 1-5% develop ATLL. Although the pathogenetic mechanisms of these two major complications likely differ, the low rates of each means that it is rare to see both sequelae in the same patient. At the Tropical Medicine Institute in Lima, approximately 70% of all cases of Norwegian scabies are associated with HTLV-1 infection and are, in the absence of any other factors, associated with immunosuppression. The lesions in this patient are highly characteristic [also in Gorgas Case 2008-08] and frequently not recognized by inexperienced clinicians used only to classic scabies lesions in normal hosts. Norwegian scabies is not responsive to normal topical agents such as benzyl benzoate or permethrin. Patients are generally treated with with ivermectin 200 µg/kg bid for 2 days which is repeated 15 days later. The prevalence of HTLV-1 in South America is generally underappreciated, normally being associated with Japanese and Caribbean populations. HTLV-1 is now known to occur worldwide, having originated in Africa. The highest prevalence is in Japan. In Perú, the disease is highly endemic (2-3% seropositivity) in Andean areas of the country, in Quechua populations who have had no contact with Japanese immigrants to the country. Other South American countries with significant rates of HTLV-1 include Brazil, Colombia, Argentina, and Ecuador. Transmission appears to be mainly vertical, with high associations with breastfeeding and duration of breastfeeding (probable route in our patient). Transfusion, sexual transmission, and IV drug abuse are much less important. The most promising intervention for aggressive disease forms has been with the use of anti-viral therapy. The combination of Zidovudine (AZT) with IFN-α, if used as a first-line treatment, dramatically increases survival in acute forms of ATLL but has no effect in lymphomatous forms [J Clin Oncol. 2009 Jan;27(3):453-9]. Because of her uncomfortable and disfiguring skin lesions our patient will receive a trial of AZT/IFN-α and if she responds this will be maintained indefinitely. Recent data has shown a 100% 10-year survival in smoldering ATLL treated with ongoing anti-retrovirals compared to a 42% 5-year survival in patients allowed to progress naturally and treated with chemotherapy in later stages of disease. Our patient has the chronic form of ATLL, analogous to chronic CLL, with cutaneous involvement, with associated, extensive, tinea corporis as well as crusted scabies, which doesn’t always require immediate treatment. However, the generalized leukemic state present required aggressive chemotherapy, which so far has responded quickly with a rapid drop in the WBC count. |