 |
Gorgas Case 2013-09 |
 |
|
Here is one last case seen by participants during the last week of the 9-week Diploma Course when the class was on a 4-day field trip to Iquitos, Perú on the banks of the Amazon River. Iquitos, with a population of approximately 400,000, is the largest city in the world that can only be reached by air or by river. The nearest road ends over 400 km away.
Publishing a case report every week for 9 weeks would not be possible without the assistance of an extremely dedicated group of people. We would like to thank in particular: Clinical Rounds Coordinator for the Gorgas Courses for case selection, coordination of case summaries and images; and of the Gorgas Center for Geographic Medicine in the UAB Division of Infectious Diseases for all publishing on the Gorgas Course web site. We hope you have enjoyed this year’s cases. In August 2013 we will be running the 2-week Gorgas Advanced Course (places are still available) and will present a couple more cases during that time. We will also be in touch in January 2014 at the beginning of next year’s case series. |
|
The following patient was seen in the outpatient department at Iquitos Hospital.
History: 46-year-old male with a two year illness that began with erythematous macular lesions on his abdomen, then the chest, the back, that later evolved into papules and nodules. Subsequently, there was involvement of his limbs, face and earlobes. The lesions are non-pruritic and painless. He denies other symptoms. No important past medical history. No history of trauma. Epidemiology: Born and lives in the jungle of Ucayali near Iquitos. No contacts with similar lesions. No known TB exposure. No sexually transmitted diseases or HIV risk factors. Physical Examination: Afebrile. HEENT: pharynx clear, normal oral mucosa. Chest clear. Abdomen: no hepatosplenomegaly or lymphadenopathy. Skin [see Images A-D]: diffuse symmetric infiltrative erythematous lesions on the skin of the face, earlobes, trunk and extremities, with multiple papules and nodules over the lesions. Loss of eyebrows and eyelashes (madarosis). Neurologic examination: on gross examination there is impairment of sensation on the lesions of the earlobes, the trunk, the ulnar aspects of both hands and the pretibial aspect of the left leg. There is thickening of both great auricular nerves, the right ulnar nerve, the left common peroneal nerve and both posterior tibial nerves. In addition, mild loss of strength in muscles innervated by both ulnar nerves. Laboratory Results: Hematology and biochemistry unremarkable. A skin biopsy was obtained [see Discussion]. 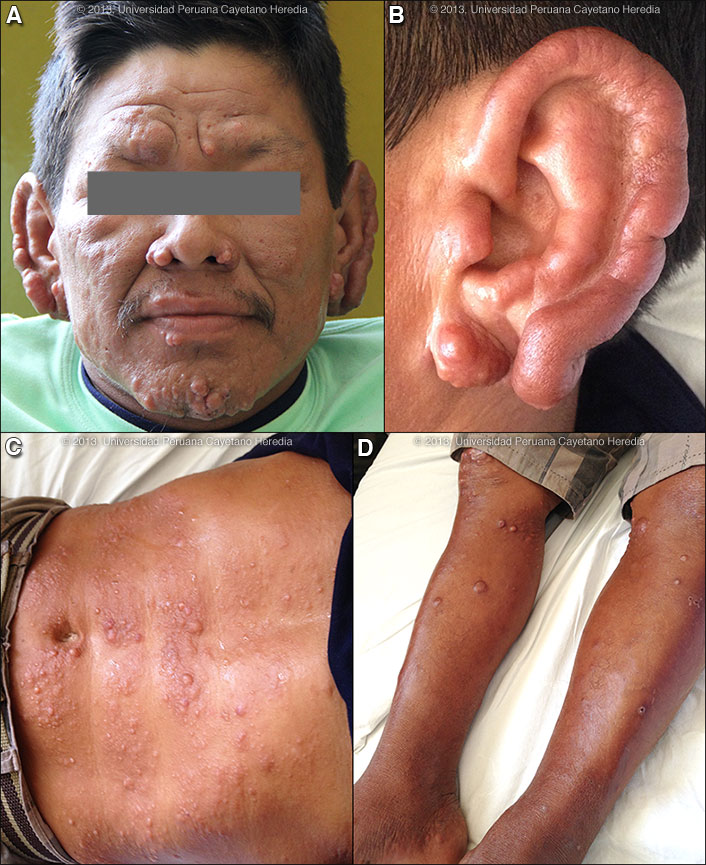
 |
|
Diagnosis: Mycobacterium leprae. Multibacillary leprosy according to the WHO classification. Lepromatous leprosy (LL) leprosy according to the Ridley-Jopling classification.
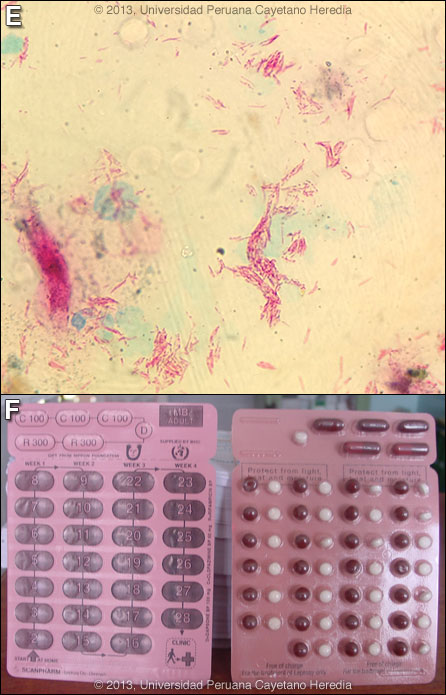
 Discussion: Slit skin smears were taken from both earlobes, elbows (laterally to avoid the olecranon). Of the 6 smears one had 4+ bacilli, four had 5+ [example in Image E] and one 6+. Slit skin smears are performed by making small (5 mm length, 2 mm depth) slits in pinched skin (to avoid bleeding), the edges of which are scraped. The material obtained is smeared on a clean slide and stained for AFB. The bacterial index ranges from zero (no bacilli in 100 oil-immersion fields) to 6+ (many clumps or globi or over 1000 bacilli in one field). As in other resource limited settings, no biopsy was performed. Leprosy is a disease of peripheral nerves and skin. Leprosy can be diagnosed clinically in any patient with simultaneous skin lesions and sensory loss over the lesions unless there is hyperkeratosis. However, in early lepromatous cases, sensation is normal over the lesions. Thus, with loss of sensation, a diagnosis of leprosy can be made; with intact sensation the diagnosis is possible but must be confirmed in some other way. This patient’s lesions are classic and typical. See Gorgas Cases 2012-02 and 2001-11 for typical skin findings in other patients. For the purposes of determining treatment, the usual and most practical grading system is the WHO classification. For choosing the regimen, it matters only whether the patient has paucibacillary or multibacillary disease. Where no slit skins smears can be done, paucibacillary leprosy is defined as five or fewer skin lesions; multibacillary cases have six or more lesions. Paucibacillary disease usually presents with small numbers of hypopigmented macules or erythematous plaques with absent or reduced sensation and well-demarcated borders. Multibacillary disease is usually widespread at diagnosis with multiple plaques or infiltrated areas of skin with indistinct borders that are often non-anesthetic, and papules or nodules. The disease can be classified precisely in the immunologic sense using the traditional Ridley-Jopling classification. This describes a spectrum of disease ranging from tuberculoid leprosy (TT) with no AFB in lesions and good cell mediated immunity, to lepromatous leprosy (LL) with many AFB and poor cell-mediated immunity. This classification is especially useful in assessing risks and prognosis. The standard WHO regimen for paucibacillary disease is 100 mg dapsone a day unsupervised and 600 mg rifampin once per month directly observed for 6 months. For multibacillary disease, the long-standing recommendation is for patients to receive 100 mg dapsone and 50 mg clofazimine a day unsupervised and 600 mg rifampin and 300 mg of clofazimine directly observed once per month. A standard WHO multibacillary dose-pack (provided free to endemic countries) is shown [Image F]; the instructions in English must be clarified for all healthcare staff and patients. WHO now recommends only 1 year of therapy for multibacillary cases [controversy discussed in Lancet. 2004 Apr 10;363(9416):1209-19], but some would treat those with high bacterial indices (4 to 6+) for the previously recommended 2 years due to higher relapse rates as we do here at our institution. The possibility of adverse effects of dapsone and clofazimine and of a Lepra reaction should always be explained to a patient who is starting treatment and a reference text should be consulted prior to initiation of therapy by anyone not familiar with these. The most common reaction in multibacillary disease, occurring in about 50% of patients with lepromatous leprosy is a Type 2 reaction, which has as the most common presentation erythema nodosum leprosum (ENL). ENL is a vasculitis at the site of any deposit of dead and disintegrating M. leprae, often accompanied by a severe systemic illness, and characterized by high levels of tissue and circulating TNF-alpha. ENL presents with fever together with many tender erythematous nodules [see Am J Trop Med Hyg. 2006;74(5):868-79]. ENL may also produce to varying degrees, neuritis, uveitis, myositis, dactylitis, periostitis, orchitis, lymphadenitis and nephritis accompanied by edema, arthralgia, and leukocytosis. ENL may occur in patients prior to therapy, during therapy and/or after therapy until the antigen load decreases markedly. ENL may present as repeated acute episodes or may be chronic and ongoing. ENL can be treated symptomatically if mild or with prednisone or thalidomide if severe [see Gorgas Case 2011-04]. In endemic areas, we usually examine the family contacts once a year for at least five years, and advise them to contact the health system in case they present any skin lesion or numbness.
|