 |
Gorgas Case 2016-11 |
 |
|
This is our last Case of the Week for 2016. We hope you have enjoyed the 2016 series of live cases each week from Perú. The Gorgas Diploma Course is held annually in February and March and we will be in touch at the beginning of next year’s case series.
Publishing these case reports would not be possible without the assistance of an extremely dedicated group of people. We would like to thank in particular UPCH Case Editors: Dr. Carlos Seas, Clinical Course Coordinator and Dr. Sofia Zavala, Associate Coordinator and UAB Case Editor: David O. Freedman, Course Director Emeritus, for case selection and coordination of case summaries and images, and Alfredo Guzman of the Gorgas Center for Geographic Medicine in the UAB Division of Infectious Diseases for all publishing on the Gorgas Course website. The following patient was seen by the Gorgas Advanced Course participants in the outpatient clinic of the Tropical Medicine Institute in Lima. Eduardo Gotuzzo and German Henostroza Course Directors 
 History: A previously healthy 25 yo male presented to the outpatient clinic complaining of multiple skin lesions for 1 month. The lesions started as small papules on the face that were unresponsive to oral acyclovir. The lesions disseminated to involve the entire body with a variety of lesions including pustules, crusted lesions, verrucous plaques and most notably ulcers with purulent discharge on the back and extremities. Fever and malaise were present during the week before presentation. He denies weight loss and fatigue. On no medication and no known allergies.
Epidemiology: Born and lives in Lima; he works as a clerk in a supermarket. He has a history of Hepatitis A at 8 years of age. MSM, multiple partners without condom use. Recent TB contact at work. Physical Examination: T 37.4o C, R 17, HR 80, BP 100/60, Sat O2 97% Laboratory Examination (on admission): WBC 9.2 (82% neutrophils, 1% eosinophils, 8% monocytes, 9% lymphocytes). Hct 36%, platelets 353,000. AST, ALT normal. Glucose 84 mg/dL. HIV ELISA positive, HTLV-1 negative, RPR negative. Chest X-ray: unremarkable. Bacterial cultures from ulcers were positive for MRSA and negative for fungi and mycobacteria.
|
|
Diagnosis: Malignant syphilis due to T. pallidum
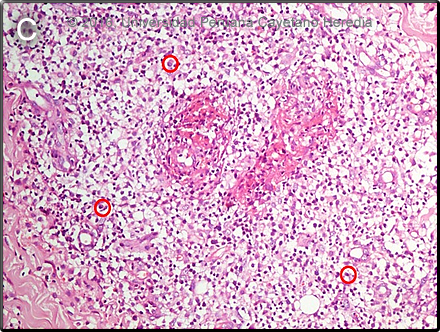
 Discussion: The patient’s serum was diluted and the repeat RPR was positive and remained positive even at a dilution >1:128. FTA-Abs was positive. This illustrates the prozone phenomenon in syphilis testing which refers to a false negative response resulting from overwhelming antibody titers which interfere with the proper formation of the antigen-antibody lattice network necessary to visualize a positive flocculation test. This phenomenon can be expected in cases of disproportionately high antibody titers, such as secondary syphilis, or with HIV coinfection. Lumbar puncture is not indicated in HIV positive patients without any neurologic findings on physical exam. Clinicians need to remain familiar with the protean manifestations of syphilis to be able to exclude the prozone phenomenon. In addition, a diagnosis of syphilis requires use of two tests: a nontreponemal test (i.e., Venereal Disease Research Laboratory [VDRL] or Rapid Plasma Reagin [RPR]) and a treponemal test (i.e., fluorescent treponemal antibody absorbed [FTA-ABS] tests, the T. pallidum passive particle agglutination [TP-PA] assay, various enzyme immunoassays [EIAs], chemiluminescence immunoassays, immunoblots, or rapid treponemal assays). In malignant syphilis, typical histopathology shows dense inflammatory infiltrate of the dermis with predominance of lymphocytes, histiocytes, and plasma cells surrounding blood vessels (Image C circles). These histological findings in isolation cannot make the diagnosis and can also be seen in leprosy and vasculitis. Special stains (not performed here), such as Warthin-Starry (silver based) and immunohistochemical stains are positive in only 57%, thus the absence of visualization of the spirochetes does not rule-out the diagnosis. Malignant syphilis is a rare clinical presentation of secondary syphilis, characterized by extensive cutaneous polymorphic lesions that evolve to ulcerative lesions with or without systemic manifestations. It was initially reported by Neisser and Hassland in 1897 in a non-HIV infected patient. The first report in an HIV infected patient was in 1988, and all recent reports of this rare condition are in immunosupressed patients. A retrospective study conducted in Germany among 11,368 HIV infected patients found that 151 patients had syphilis (1.3%) and that 11 (7.3%) of them had malignant syphilis [Schofer H. Genitourin Med 1996;72:176-81]. The condition is mostly seen in males, mean age is 32 years. Interestingly, 80% of patients in a study of 21 HIV infected-patients had CD4 cell counts above 200 cells, 33% had ocular involvement, and 24% developed oral lesions that our patient did not have [Romero-Jiménez M. An Med Interna 2003;20:373-6]. The diagnosis is usually made taking into account the distinctive cutaneous clinical manifestations, positive serology, pathological findings and response to treatment, which is usually quick. In the tropics especially, the differential diagnosis is broad and includes: Treatment is with benzathine penicillin, dose and duration have not been studied. Most reports suggest that 2.4 million units per week for 3-4 weeks is adequate. As expected, lesions improved quickly after treatment in our patient, and no Jarisch-Herxheimer reaction, as can be seen in syphilis, occurred. We would like to thank: Francisco Bravo, Dermatology Faculty |