 |
Gorgas Case 2017-08 |
 |
|
The patient was seen in the Internal Medicine Service of the Cayetano Heredia National Hospital in Lima, Peru.
 History: 32-year old male presented to the ED with 8 months of abdominal pain and bloody diarrhea. The illness began with colicky mid-abdominal pain with 4/10 intensity, 3 times per day. 5 months before presentation liquid stools 2-3 times/day without mucus or blood began. Symptoms progressed and by 3 months before presentation the abdominal pain increased to 7-8/10 and he was having 5-6 bloody stools per day, associated with anorexia and weight loss of 10 kg. A colonoscopy and biopsy 1 month prior to presentation resulted in a diagnosis of Crohn’s disease and treatment with steroids and sulfasalazine without improvement.
One month before presentation, intermittent fever, productive cough, pallor, palpitations, dyspnea and fatigue led to his presentation to us. He denies any skin or mucosal lesions. Past medical history relevant for a diagnosis of external hemorrhoids on 2016, treated with topical creams. No surgeries or previous hospitalizations. Epidemiology: Born and currently living in Moyobamba, a city in the high jungle, in a house with running water but no electricity or sewage, no animals at home. He works at his farm since age 16 and has coffee and rice crops, cattle, pigs and dogs. 3 years ago, one of his cows died of anthrax; he did not perform an autopsy. Physical Examination: BP 120/80 mmHg, HR 117, RR 19, afebrile, SO2 98%, FIO 21% Laboratory: CBC: Hb 5.6, Hct 19%, mycrocitic, hypochromic. WBC 12.0 (0 bands, 73 segmented neu, 1.1 eos, 0.1 baso, 8.1 mono, 17 lymph). Platelets 767 000. ESR 49, CRP 96.
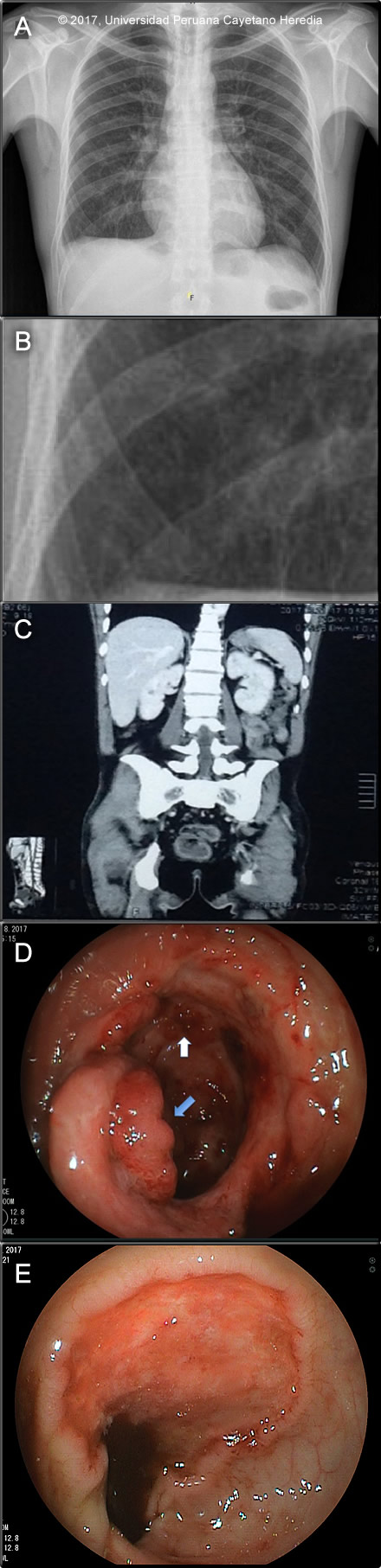
Glucose 72 mg/dL, urea 21.9 mg/dL, crea 0.7 mg/dL. Ca total 7.8 mEq/L, Na 136 mEq/L, K 4.08 mEq/L, Cl 106 mEq/L. Total prot 4.8 g/dL, alb 2.2 g/dL. AST 18 U/L, ALT 52 U/L, AP 68 U/L, GGT 32 U/L, LDH 346 U/L. Normal bilirrubins. Stools for ova and parasites: Negative. Serology for HBsAg, HIV and HTLV-1: negative. Sputum AFB: negative PPD: 0mm Chest X-ray (Image A and B), abdominal CT (Image C), and colonoscopy (Image D; ileocecal valve) and (Image E; colon) are shown. UPCH Case Editors: Carlos Seas, Clinical Course Coordinator / Sofia Zavala, Associate Coordinator UAB Case Editor: David O. Freedman, Course Director Emeritus / German Henostroza, Course Director |
|
Diagnosis: P. brasiliensis, Chronic multifocal form
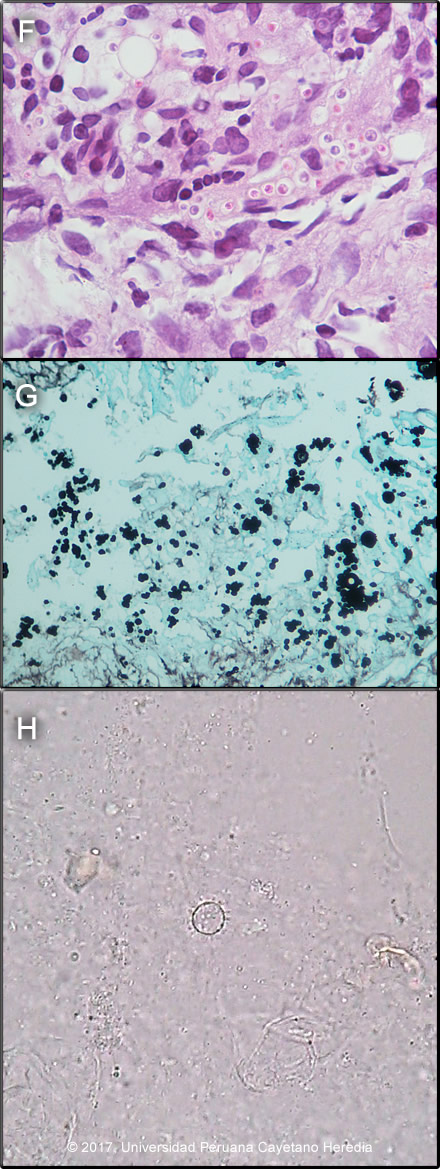
 Discussion: On biopsy of colonic lesions, a dense chronic inflammatory reaction with granuloma formation with yeast forms of varying sizes, with some yeast chains within and outside of multinucleated giant cells was observed [Image F]. A Grocott stain showed yeast cells of different sizes with peripheral budding [Image G]. A touch prep of one of the colonic biopsies identified yeast cells typical of P. brasiliensis in a KOH preparation. Subsequent sputum, urine and stool samples tested positive for yeast cells in KOH preps. Image H shows a mother cell with multiple peripheral daughter cells mimicking a pilot´s wheel typical of P. brasiliensis. The CXR was reported as suggestive of micronodular involvement [Image A and B], no chest CT scan is available. Hepatosplenomegaly is the main finding on the CT abdomen [Image C]. The colonoscopy disclosed punched out ulcers with raised edges and a fibrin background at 15, 10 and 5 cm from the ileocecum valve, the valve itself looked edematous and erythematous, with erosions and small ulcers [Image D]. The cecum showed an eroded mucosa with loss of the normal vascular pattern [Image D]. Multiple longitudinal ulcers with irregular and edematous edges on a fibrin base, some of them with necrotic areas and spontaneous bleeding, were seen along the rest of the colon [Image E]. Punched out ulcers were observed in the rectum. The upper endoscopy was normal. The diagnosis of Crohn´s disease was unlikely in this patient based on the epidemiology, rarity of this disease among Peruvians, but mostly on the lack of response to treatment and on infrequent clinical manifestations for Crohn´s disease seen in this case, such as generalized lymphadenopathy and lung involvement. The chronic form of paracoccidioidomycosis most often involves pulmonary disease with oral mucosal involvement as a frequent complication [Gorgas Case 2004-05]. The differential diagnosis for the lung disease includes: TB, histoplasmosis, lymphoma, cancer and cryptococcosis. The typical radiographic pattern of paracoccidioidomycosis is with bilateral mixed infiltrates (alveolar and interstitial), mainly located in the middle and lower lobes. Interstitial lesions may have miliary (as in this case), nodular or fibronodular patterns. Other patterns observed in these patients are hilar and mediastinal lymph node enlargement, cavities, and calcified lesions. Extrapulmonary disease is found in over 70% of cases and may involve skin, mucous membranes, lymph nodes, adrenals, abdominal organs and CNS (in 9-25%). Gastro-intestinal seeding in paracoccidioidomycosis results from disseminated abdominal lymph node involvement [Gorgas Case 2009-10]. It is rarely recognized in life due to nonspecific clinical manifestations that can resemble other conditions such as amebiasis, balantidiasis [Gorgas Case 2002-07], tuberculosis, cancer or inflammatory bowel disease, as in this case [J Clin Gastroenterol 2011;45:87-91]. Ulcers due to typhoid fever are usually in the ileum or proximal colon and would be preceded by a progressive febrile illness over weeks without diarrhea [Gorgas Case 2009-04]. Involvement of the entire gastrointestinal tract has been reported, from the esophagus to the rectum. However, small and large intestine involvement is most commonly reported. Autopsy studies documented 10-30% of intestinal involvement; the ileocecal segments are the most commonly affected areas Ano-rectal disease is reported in 2% [Rev Soc Med Trop 2001;34:583-6] [Gorgas Case 2005-12]. The disseminated disease observed in this case with pulmonary, lymph node and gastrointestinal involvement might have resulted at least in part due to iatrogenic use of steroids. Paracoccidioidomycosis, also known as South American blastomycosis, is found in humid forested or lush green areas of the Americas from Southern Mexico south to Uruguay and Argentina. It appears to be most common in Brazil. The exact habitat of the organism is unclear but transmission is most often described as being entirely by airborne inhalation. Travelers spending less than 6 months in an endemic area are unlikely to acquire paracoccidioidomycosis. |