 |
Gorgas Case 2017-07 |
 |
|
The patient was seen in the intermediate neonatal care unit of the Cayetano Heredia National Hospital in Lima, Peru.
 History: A 23-day old preterm infant with an estimated gestational age of 32 weeks and a birth weight of 1360g, delivered at home from a 19 year-old mother (G3P2) without prenatal care, presented sudden onset tachycardia, fever, respiratory distress with borderline desaturation while being admitted at the intermediate neonatal care unit. He was initially brought by his family to the ED 2 hours after delivery with respiratory distress and hypoglycemia and was subsequently treated in intensive care with 5-days of antibiotics until neonatal sepsis was ruled out. He improved gradually and was tolerating room air until this sudden deterioration for which he was readmitted to the Neonatal ICU for oxygen support and further testing.
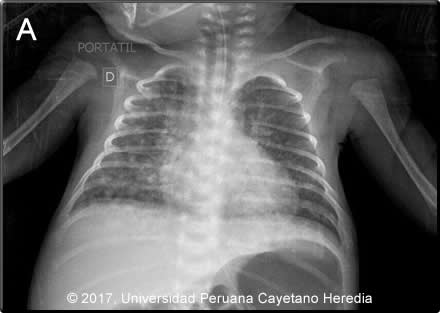
Epidemiology: Product of an uncomplicated pregnancy, dates unknown. UTI treated with vaginal medication 1 week prior to delivery. Two days of contractions with spontaneous rupture of membranes 12 hours before vaginal delivery. As reported by midwife, amniotic fluid was clear, placenta intact and completely expelled. Anthropometrics were all adequate for his estimated gestational age of 32 weeks. Immediately post-partum, the mother was found to be tachycardic, febrile and with vaginal bleeding and underwent puerperal curettage. She did not directly breast feed her infant during the hospitalization. Mother lives in San Juan de Lurigancho, Lima. Housewife, no risk factors for HIV infection, no history of recent travels. Physical Examination: HR 174, RR 58, T 36.8ºC, sO2 91% (FiO2 0.21). Moderately ill infant with respiratory distress. Skin: warm, dry, mild pallor. Capillary refill less than 2 seconds.Lungs: symmetrical chest, subcostal retractions. Normal breath sounds, no crackles..Heart: regular rate and rhythm, no murmurs. Abdomen: Distended, bowel sounds present. Liver 1cm below right costal border. Neurologic: somnolent, decreased reactivity to tactile stimuli. Axial and appendicular hypotony, weak suction. Laboratory: Hb 12.5 g/dL, Hct 35%. WBC 21.6 (2 bands, 54 neutrophils, 4 basophils, 1 eos,, 11 monos, 25 lymphs). Platelets 386 000. Blood type: O +, Mother: O+. Urea 16 mg/dL, creatinine 0.5 mg/dL. Na 137 mEq/L, K 5.04 mEq/L, Cl 102 mEq/L. AST 19 IU/L, ALT 15 IU/L, AP 365 IU/L. ABG: pH 7.347, pCO2 35.1, pO2 78.9, sO2 97.5%, HCO3 18.7. Urinalysis: WBC 0-3/hpf, RBC 0-2/hpf, few epithelial cells. Lumbar puncture: WBC 2/hpf (100% neutrophils), RBC 300/hpf, glucose 43, protein 171. Gram stain: negative. PPD: negative. Abdominal ultrasound: liver was normal, no hydronephrosis, no free fluid in the abdominal cavity. Chest X-Ray (see Image A).
UPCH Case Editors: Carlos Seas, Clinical Course Coordinator / Sofia Zavala, Associate Coordinator UAB Case Editor: David O. Freedman, Course Director Emeritus / German Henostroza, Course Director |
|
Diagnosis: Mycobacterium tuberculosis, congenital form.
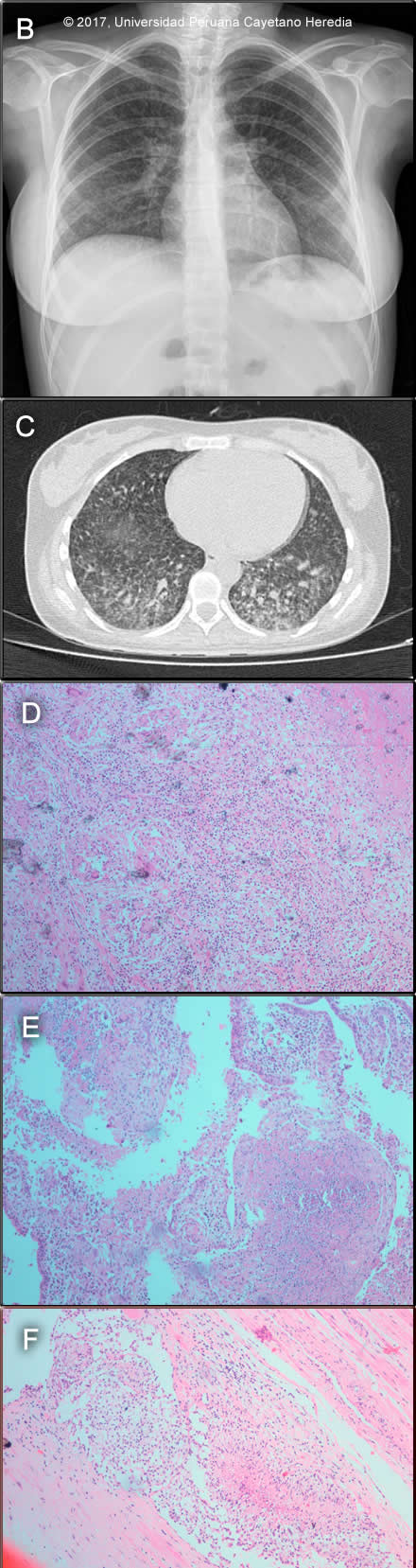
 Discussion: On repeat testing, a gastric aspirate from the infant was positive for AFB (3+). Mother and baby were both HIV negative. Investigation of the mother, who remained febrile after the curettage, included chest X-ray and CT (Image B, C) showing a diffuse micronodular pattern. A pelvic CT (not shown) showed a large heterogeneous uterus which on examination after hysterectomy with bilateral salpingectomy, showed a chronic granulomatous process with giant multinucleated cells in the endometrium, myometrium (Image D) and Fallopian tubes (Image E). In addition, vascular emboli of tissue with granulomatous reaction in the parametrium (Image F) were seen though Ziehl-Neelsen stain was negative. The mother remained febrile after surgery. The diagnosis of miliary tuberculosis in the mother with genital involvement and the finding of AFB in the child led to the diagnosis of congenital tuberculosis and the need to start antituberculous therapy (RIPE) in both. Congenital tuberculosis is the perinatal transmission of M. tuberculosis. It is thought to be acquired in any of the following ways: transplacentally, where the primary complex is found in the liver; by aspiration of infected amniotic fluid during birth, with the lungs as the primary focus, or ingestion of infected amniotic fluid, where the primary infection site is in the gut. [N Engl J Med. 1994; 330:1051–4]. The differential diagnosis in a newborn presenting with this clinical syndrome should include neonatal sepsis, toxoplasmosis, rubella, CMV, HSV (TORCH) , other congenital infections consider within the TORCH complex as others (O) including Syphilis, Parvovirus B19, VZV; HIV. In preterm newborn with respiratory distress consider hyaline membrane syndrome (respiratory distress syndrome). The Cantwell criteria for congenital TB are: Although in our case, there was no evidence of a liver primary complex on ultrasound, the presence of genital tuberculosis in the mother supports also transplacental acquisition of MTB. The diagnosis of tuberculosis in an infant is based on a TST result, which is often negative, and a chest radiograph or other radiologic studies in a patient with a compatible clinical syndrome. Microbiological confirmation should be made whenever possible by examining specimens such as gastric aspirate, ascitic fluid, endotracheal aspirate, middle ear fluid, and CSF [Pediatrics 1980;66:9804]. |