 |
Gorgas Case 2016-01 |
 |
|
The Gorgas Courses in Clinical Tropical Medicine are given at the Tropical Medicine Institute at Cayetano Heredia University in Lima, Perú. For the 16th consecutive year, we are pleased to share interesting cases seen by the participants that week during the February/March course offerings. Presently the 9-week Gorgas Course in Clinical Tropical Medicine is in session. New cases will be sent by e-mail every Tuesday/Wednesday for the next 9 weeks. Each case includes a brief history and digital images pertinent to the case. A link to the actual diagnosis and a brief discussion follow.
David O. Freedman, Eduardo Gotuzzo, German Henostroza
Course Directors |
|
The following patient was seen in the inpatient department of the 36-bed Tropical Disease Unit at Cayetano Heredia National Hospital in Lima, Perú.
 History: 17 year-old male admitted for further evaluation of fever of unknown origin. The patient reports illness onset 4-months earlier with malaise, fever and prominent night sweats. Two weeks later he noticed painless, erythematous, papular lesions on the chest wall that progressed over 2 days to the arms and legs and 1 week later the presence of generalized lymphadenopathy (inguinal, axillar, retro-auricular and cervical), and significant weight loss (12kg). Extensive work-up for infectious disease and malignancy was unrevealing and he was started on 4-drug anti-TB treatment 2 months prior to admission. Due to intolerance and no improvement he stopped it after 40 doses and presented to us. No past medical history and no current medications.
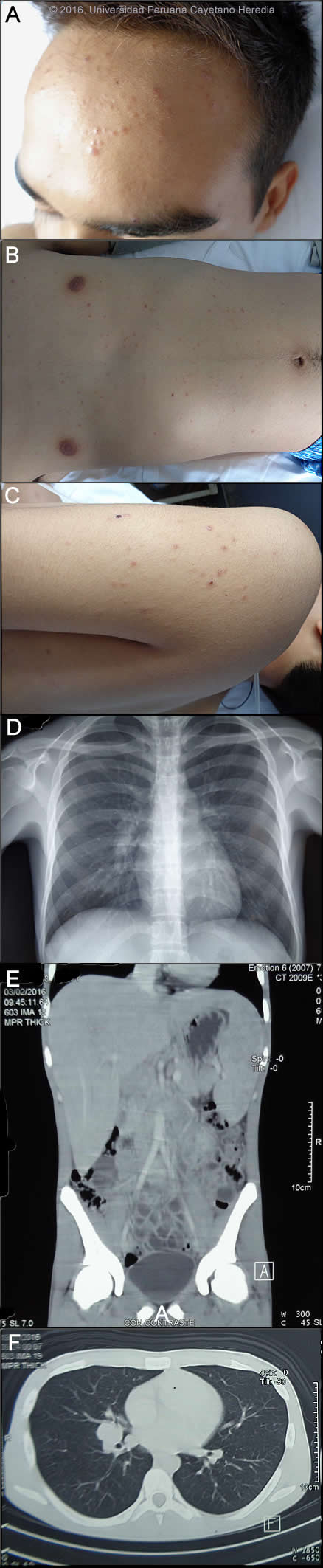
Epidemiology: No medications, no known drug allergies. Family history is not significant. Student, born and lives in Tarapoto, a low jungle area of Peru. He has a cat at home and participates in motocross only within the city. Non-smoker, occasional alcohol consumption. Heterosexual, with 4 lifetime partners with regular condom use. No recent travel outside his city. No known TB contact. Physical Examination: HR 101x’, RR 18x’, BP 100/60, T37.8C. Alert & oriented. General pallor, multiple papular lesions, some of them umbilicated, located on the face, trunk and extremities [Images A,B,C]. No mucosal lesions. Multiple mobile, soft, non-tender lymph nodes 1-2 cm in the cervical, axillary and inguinal chains with no external drainage. Lung and CVS: normal examination. Abdomen: Normal bowel sounds, non-tender to palpation, liver 4 cm below right costal margin, mildly painful to deep palpation; spleen 4cm below left costal margin. Normal neurologic exam. Laboratory Examination (on admission): Hb 9.9, Hct. 30, WBC 8.2 (61 neutrophils, 0 bands, 12 lymphs, 4 monos, 23 eosinophils), 413,000 platelets. Bilirubin, liver and renal function normal. CRP 33.5 mg/dl. HIV, RPR, brucella agglutinins negative. Chest x-ray, CT chest, and CT abdomen are shown in Images D,E,F.
|
|
Diagnosis: Paracoccidioidomycosis, juvenile form.

 Discussion: Direct KOH preparation of a skin lesion was positive for yeast structures compatible with Paracoccidioides brasiliensis showing spherical cells 10-40 microns in diameter with a thick birefringent cell wall surrounded by several peripheral buds characteristic of Paracoccidioides brasiliensis [Image G]. When completely surrounded by buds a so-called “pilot-wheel” pattern occurs. Culture and serology are pending. Biopsy of a cervical lymph node showed granulomatous lymphadenitis without multinucleated giant cells or central necrosis. Fungal stains are pending. PCR for TB performed twice gave inconclusive results. Direct scrapings or aspirates will be positive in the vast majority of cases of paracoccidioidomycosis with cutaneous lesions. Chest X-ray interpretation: right hilar lymphadenopathy without pulmonary infiltrates. Chest CT interpretation: mediastinal and right hilar lymphadenopathy. Abdominal CT interpretation: hepatomegaly and splenomegaly with no focal lesions, retroperitoneal and mesenteric lymphadenopathy, free peritoneal fluid. The constellation of clinical and laboratory findings in this patient points towards juvenile paracocci more than to TB; skin lesions, visceromegaly and generalized lymphadenopathy with no mucosal or lung involvement plus eosinophilia are the hallmarks of this entity. Other possible conditions to be included in the differential are infectious conditions such as histoplasmosis (only unusually presents this way in a immunocompetent host), cryptococcosis (absence of lung-meningeal involvement and no immunosuppression makes it less likely); visceral leishmaniasis (not endemic in Peru, but skin lesions and eosinophilia are not characteristic of it); brucellosis (skin lesions and generalized lymphadenopathy with no articular involvement and negative serology makes it unlikely); infective endocarditis (no murmur and evidence of other embolic lesions); EBV, CMV and other viruses including acute HIV are less likely as well, and malignancy (lymphoma in particular). Chronic bartonellosis due to B. bacilliformis infection can cause fever, anemia, splenomegaly, and similar diffuse skin lesions [see Gorgas Case 2005-8]. Paracoccidioidomycosis is most often an indolent and relapsing disease causing chronic pulmonary and mucosal manifestations. The chronic form (adult type) of the disease is believed to represent reactivation of latent infection initially acquired via inhalation. The chronic forms represent approximately 94% of all cases in the experience at our institute (94 patients, up to 2001), and approximately 85% in the Brazilian series [Rev Soc Bras Med Trop. 2003 Jul-Aug;36(4):455-9]. See examples of this in Gorgas Cases 2005-12, 2009-06, and 2004-05. We have also previously shown a case of the chronic progressive form of the disease [Gorgas Case 2003-07]. This current case is representative of the relatively uncommon “juvenile” acute progressive and disseminated form of the disease, which usually (but not always) affects adolescents and young adults. After an initial inhalation event [Clin Infect Dis. 2005 Jan 1;40(1):e1-4] which is usually self-resolving, the reticuloendothelial system is widely affected. Diffuse lymphadenopathy, hepatosplenomegaly, and papular skin lesions with a large burden of yeast forms in all tissues as in our patient are usual clinical manifestations. The course is rapidly progressive over weeks in contrast to months or years for the chronic progressive forms. Early on in juvenile disease, CT imaging of the chest reveals changes consisting of mediastinal and hilar adenopathy and interstitial infiltrates [Semin Respir Crit Care Med. 2008 Apr;29(2):182-97]. The respiratory system and mucosal surfaces are not usually involved in the clinical manifestations of the acute juvenile disease as they are in the chronic forms. However, Gorgas Case 2010-7 shows an instance of very long-standing disease with the juvenile form which includes pulmonary involvement. The juvenile patients manifest with an antigen specific depressed cell mediated immune response to paracoccidioidal antigens in vitro and with negative skin tests. Responsiveness to mitogens and other antigens is normal. In vitro, patients have a predominant Th2 cytokine pattern. Paracoccidioidomycosis, also known as South American blastomycosis, is found in humid forested or lush green areas of the Americas from Southern Mexico south to Uruguay and Argentina. It appears to be most common in Brazil. The exact habitat of the organism is unclear but transmission is described as being entirely by airborne inhalation. Primary pulmonary infection may be asymptomatic and self-limited, but even with treatment will produce at least moderate pulmonary fibrosis. Our patient is unusual in being one of the few to report no rural jungle exposure [Braz J Infect Dis 2010;14(1):77-80]. His motocross sport activity, however, implies deep exposure to soil and took place within the city but outside of usual urban settings. Rural adult male agricultural workers between 30-60 years of age are most affected by the infection. Travelers spending less than 6 months in an endemic area are unlikely to acquire paracoccidioidomycosis. Sulfonamides, ketoconazole, itraconazole, and amphotericin B are all effective therapies. Amphotericin should be reserved for severe cases such as this one. For milder cases, itraconazole 100-200 mg/day for 6-9 months is regarded as the treatment of choice for both the juvenile and chronic forms when it is available and affordable. In the present case, amphotericin B was started at 0.7 mg/kg/d, the plan in to give 2-3 weeks depending on clinical response, to be switched after that to itraconazole 200mg/d per at least 1 year. Follow-up requires measurement of serum drug levels of itraconazole at least one, and clinical and mycologic evaluation (if there is something to sample). The fever in this patient resolved on day 4 of Amphotericin and he has begun to gain weight. Relapses are common with less than 6 months therapy and expert opinion is now that 1 year is not necessary. In the developing-world setting, ketoconazole is likely equally effective and is usually less than half the cost. However, 12 months of therapy with ketoconazole (or sulfonamides) is generally recommended. Brazilian guidelines recommend measuring serologic titers of IgG that correlate with disease activity and offer treatment for a total duration of 2 years after normalization of serum titers, but this is not evidence-based.
|