 |
Gorgas Case 2025-6 |
 |
|
The following patient was seen in Cuzco by the 2025 Gorgas Course participants.
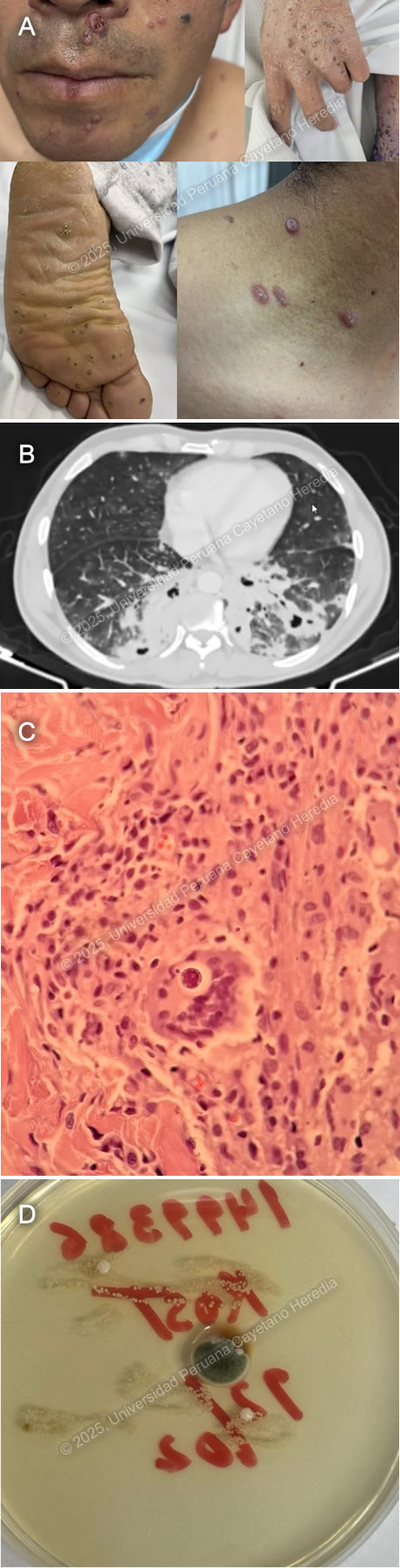 History: A 43-year-old male patient presented to the emergency department at Cuzco with a 6-month history of productive cough, fever and 3 months of disseminated cutaneous lesions. Six months before admission the patient presented productive cough with blood-tinged sputum, subjective fevers and night sweats. Symptoms persisted and 3 months before admission multiple umbilicated papules first appeared in the palms and soles and progressed to affect the rest of the body. Lesions were painful, non-pruriginous and had no discharge. Three days before admission he developed shortness of breath for which he attended the ED and was admitted. Epidemiology: The patient was born in the city of Cuzco and worked as an agricultural technician. He lived with his female partner, denied polygamy, MSM or contact with sexual workers. He traveled to the low jungle in two occasions, 1 year and 7 months, before admission where he had significant exposure to animals including birds and bird guano. Physical Examination on admission: BP: 120/70 mmHg; RR 26; HR 91; T: 36.5°C, Sp02 92% on room air. He appeared to be tachypneic and in mild respiratory distress. On the skin, multiple erythematous umbilicated papular lesions on the palms, soles, upper and lower extremities, trunk, face and tongue were noted (Image A). There was no palpable lymphadenopathy. There were decreased breath sounds bilaterally with bibasilar crackles. The rest of the exam was normal. Laboratory: WBC 12,910/µL with Seg 10,700 (82.9%), Lin 1,110 (8.6%), Mon 750 (5.8%), Bands 0.9%; Hb 12.6 g/dL with MCV 76.1 fL, MCH 25.7 pg; Platelets 332,000/µL, CRP: 19.44 mg/L. Creatinine 0.91 mg/dL, Urea 40.9 mg/dL, AST 34 U/L, ALT 73 U/L, TB 7.2 mg/dL (DB 1.79 mg/dL), Alk. Phos 298 U/L, GGT 335 U/L. Na+ 139 mmol/L, K+ 5.4 mmol/L. TSH 1.91 µIU/mL, free T4 1.45 ng/dL, T3 0.26 ng/mL. HIV, HTLV-1, VDRL, HBsAg, anti-HBc, HCV, HAV were negative. Anti-MPO (ANCA P), Anti-PR3 (ANCA C) negative. Blood cultures came back negative, as well as AFB sputum, urine, and stool. Sputum GeneXpert was negative, but a BAL sample GeneXpert was positive for MTB with indeterminate rRifampicin resistance. Imaging: A CT chest revealed alveolar consolidation in the right lower lobe with peripheral air bronchogram along withnd other scattered ground-glass opacities in both lungs and in the left lower lobe, cavitary-appearing lesions with peripheral alveolar consolidation (Image B). Both head and Abdominopelvic CT were normal. Pathology: : A skin biopsy (Image C, H&E stain) and culture (Image D) from the lesions were performed, revealing the following structures. UPCH Case Editors: Carlos Seas, Course Director / Mario Suito, Associate Coordinator |
|
Discussion: Histopathology revealed budding yeasts and culture demonstrated fungal colonies compatible with Cryptococcus sp. Cryptococcosis is caused by the ubiquitous yeasts of Cryptococcus neoformans, C. gattii, and, less commonly, C. laurentii and C. albidus. C. neoformans is most commonly isolated from soil contaminated with bird (pigeons, turkeys and chickens) guano. Humans are infected after inhalation of the Cryptococcus sp. Propagule, which in normal hosts is eliminated, but in certain cases and more frequently in immunosuppressed patients, can proliferate and cause invasive disease. Of all affected patients, 80-85% have a predisposing condition, the most common being HIV infection (1). Although less frequently affected, the remaining 20-25% of non-HIV and non-transplant (NHNT) patients have more lung involvement, higher mortality (2), and longer duration of symptoms (34 days vs 81 days, p < 0.001) (3). Pulmonary involvement is the second most common location after CNS and includes well-defined single or multiple parenchymal nodules, masses, parenchymal infiltrates, hilar lymphadenopathy, pleural effusions, and cavitary lesions (4). Cutaneous cryptococcosis almost exclusively represents disseminated disease and is the third most affected organ with protean manifestations. Papules with an ulcerated center are the most common manifestation and may resemble the umbilicated papules of molluscum contagiosum (5). Diagnosis involves either direct observation of the encapsulated yeasts, culture and antigen detection. Classically, the use of the inverse contrast staining of India ink has been used with high specificity (100%) low sensitivity in non-HIV (50%) compared to moderate to high (80%) in HIV infected patients (4). Yeasts surrounded by apparently empty spaces may be seen in H&E stains from affected tissues. The polysaccharide capsule can by identified with mucicarmine and alcian blue stains and the yeasts as well as the narrow budding can be identified using silver fungal stains such as Gomori methenamine stain. Culture from CSF and peripheral blood can give positive results in 3-7 days and the quantitative analysis of the colony count can be used to evaluate antifungal therapy effectiveness. Glucuronoxylomannan (GXM) polysaccharide antigen detection using the latex agglutination test is highly sensitive and specific when used in serum and CSF. Recently, a cheap, rapid, and simple lateral flow assay (LFA) has been developed with comparable test characteristics, widely replacing latex agglutination in routine clinical practice (6-9). Antigen titer measurement is inaccurate and should not be used for treatment decisions. Treatment of non-CNS cryptococcosis is extrapolated from CNS data. Induction therapy with liposomal amphotericin B (3-4 mg/kg IV) daily plus flucytosine (100 mg/kg PO daily in four doses) should be continued for at least 2 weeks. Before switching to consolidation therapy, the patient should have clinical improvement and CSF sterilization, the latter being demonstrated by a repeat LP for fungal culture at the 2-week mark before switching to Fluconazole 400-800 mg PO daily consolidation therapy for at least 8 weeks, after which patients can be switched to maintenance therapy with Fluconazole 200mg PO daily for at least 1 year (10, 11). In cases of CNS Cryptococcosis, management of increased intracranial pressure with either repeat LP’s or lumbar drain decreases mortality and should be pursued aggressively (12). Our patient was started on both antifungal and drug-sensitive tuberculosis treatment. GeneXpert Ultra detects M. tuberculosis (LOD: 16 CFU/mL) and rifampicin resistance (LOD: ~100 CFU/mL) via rpoB mutations. In trace-level paucibacillary TB, resistance cannot be determined, requiring confirmation with MGIT culture or Line Probe Assays (13). References |